Testing, contact tracing, and quarantining infected people are all tools in the effort to mitigate the spread of Covid-19. So are mask-wearing and social distancing. But what impact does each have? A study co-authored by MIT researchers finds that robust testing, contact tracing, and quarantining by household can keep cases within the capacity of the health-care system — preventing a “second wave” — while allowing for the reopening of some economic activities.
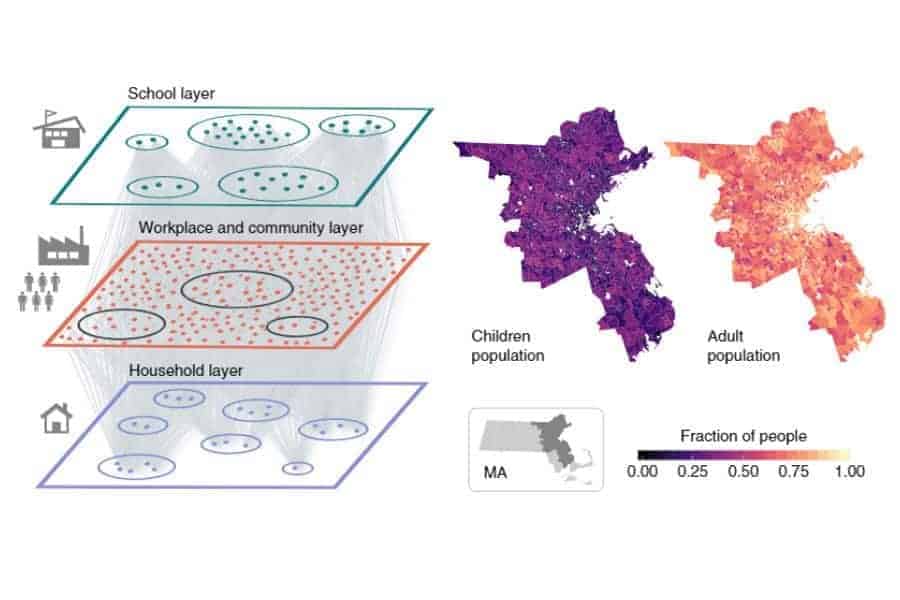
The paper, published Aug. 5 in Nature Human Behaviour, details a novel model that integrates anonymized, real-time mobility data with census and demographic data to map Covid-19 transmission in the Boston, Massachusetts area. The authors include Esteban Moro, a visiting research scientist in the MIT Media Lab and MIT Connection Science, and Alex “Sandy” Pentland, director of MIT Connection Science and a professor in the Media Lab and the Institute for Data, Systems, and Society (IDSS).
This research sheds new light on possible pitfalls and solutions as cities look to lift restrictions that have been in place throughout the summer in many locations. Using data from approximately 85,000 people in the greater Boston area, combined with known information about Covid-19 transmission rates, duration of stages, and other data points, the authors’ model forecasts the number of new cases and hospitalizations under various scenarios of lifted restrictions.
“If we want to re-scale our lives, economy, and cities, we need to understand better how the infection is spreading across people and communities,” says Moro. “Shutting down the whole economy and our cities because of a second wave might not be needed if we include accurate information about how people are behaving, moving, shopping, et cetera in our society.”
In establishing a baseline, the study found that unmitigated lifting of restrictions would likely lead to a “second wave” that would quickly overwhelm Boston’s health-care facilities, with peak of daily incidence of 25.2 newly infected individuals per 1,000 people, leading to a need for about 12 times the available intensive-care unit (ICU) beds.
A second scenario, referred to as LIFT, assumed an additional eight weeks of stay-at-home order, followed by another four of partial reopening, including work and community spaces, but not full reopening of restaurants and other spaces with mass social gatherings. After the total 12-week period, there would be a full lifting of all restrictions. In the LIFT scenario, the modeled impact was still well beyond the capacity of health-care facilities, with a need for over nine times the ICU beds available at the peak of the likely second wave.
It might be that only a safe, effective, and widely distributed vaccine will allow the world to return to life as usual. However, the authors propose a third scenario — called LET, short for Lift and Enhanced Tracing — that keeps cases and hospitalizations manageable while allowing for a wide return to work and social activity.
The LET scenario involves the same LIFT measures, but adds robust testing, contact tracing of symptomatic people, and quarantining of all household members of people who came in close contact with someone who tests positive for the virus. After lifting restrictions, at rates of 50 percent detection of positive cases within two days of onset of symptoms, tracing of 40 percent of contacts, and quarantine of all household members of those contacts, the model shows just 0.29 people per thousand in hospitals per day, compared with more than five per day under LIFT measures alone and more than seven under the unmitigated scenario. ICU beds would be more than adequate at all times under this scenario.
The advantage of whole-household quarantine is that it simplifies contact tracing, working at the level of small groups of people, rather than individuals. Followup calls to check for compliance would also be streamlined. Furthermore, the model assumes no additional precautions, such as masks and social distancing. Therefore, it is expected that new cases and hospitalizations could be even lower if people were to continue some of the practices that have helped combat the spread of Covid-19 thus far.
This approach is not without sacrifice. Quarantining full households presents unique challenges — it might be hard for quarantined families to obtain necessities, and quarantining together with others with known risk of infection may not be desirable. The study notes that at the peak, with 40 percent contact tracing, as many as 9 percent of all people in the city could be under quarantine. However, this number would gradually decline to around 3 percent. The total number in quarantine could be further reduced if testing ramps up more significantly. The authors suggest that the trade-off of higher numbers of people in quarantine compared with the massively disruptive long-term social isolation policies that would otherwise be needed to keep new infections manageable is well worth it. Life could return to some degree of normalcy, and the economy could begin to recover.
Since the study was carried out, Massachusetts has moved toward a manual tracing strategy in which thousands of people have been hired to trace potential infections. Moro explains that this could work if the number of cases is small and controlled, but it might be insufficient if the number of cases scales up. He also notes that hiring contact tracers has been problematic. He suggests a possible solution to deal with sudden growth in the number of cases: combine manual and digital contact tracing via an app.
The model used in the study will continue to be developed and enhanced, and the authors plan to examine other cities beyond Boston. They will use real-time behavior data to investigate how infection is actually propagating and detect when, where, and why spreading events are happening.
MIT Connection Science is a research group hosted by the Sociotechnical Systems Research Center, a part of IDSS.