For two decades, the number of Americans who die each year from drug overdoses has steadily risen, from less than 20,000 in 1999 to more than 80,000 in 2020. By studying patterns of these drug-related fatalities, researchers at University of California San Diego School of Medicine, San Diego State University (SDSU), and international collaborators have designed and validated a prediction model to signal counties at risk of future overdose death outbreaks. The goal of the open-source tool is to predict and prevent deaths through early deployment of public health resources.
Findings were published June 9, 2021 by Lancet Public Health .
“A big challenge for public health experts is figuring out which parts of the country are at greatest risk of future overdose outbreaks. If we can predict where such outbreaks may happen, then we will be empowered to intervene and stop deaths from occurring,” said senior author Annick Borquez, PhD, an epidemiologist and assistant professor in the Division of Infectious Disease and Global Public Health at UC San Diego School of Medicine.
The opioid epidemic has been described as an overlapping triple wave of fatal overdoses due to prescription opioids, heroin and highly potent synthetic opioids, including fentanyl. The investigators used this third wave to investigate whether a tool could be developed to predict and prevent deaths.
“This study provides a novel, rigorously validated tool to inform policy planning in the context of overdose epidemics driven by emerging drugs and sets a new standard for the development of a data-driven response to drug use epidemics,” said first author Charlie Marks, MPH, graduate research assistant, SDSU-UC San Diego joint doctoral program in Interdisciplinary Research in Substance Abuse.
Using CDC data from 2013 (when the fentanyl epidemic began) up to 2018 (the most recent data available at the time), the research team designed and trained a retrospective statistical model to find patterns in the relationship between county characteristics and overdose deaths, then used the data to predict fatality rates in the next year. The predictions were then compared with actual overdose death rates in each county.
“We found that our approach brought substantial improvement to predicting counties with high fatal overdose rates compared to a simple benchmark that relied on past year rates alone. We also found that increased overdoses in a neighboring county are very predictive of future overdoses in a given county, indicating that the overdose epidemic spreads geographically,” said Marks.
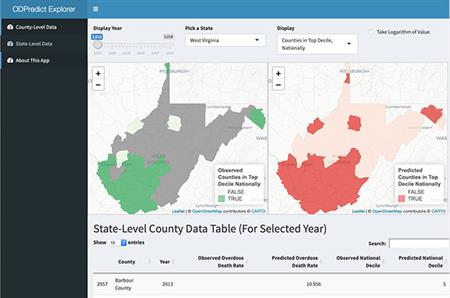
The team developed the OD Predict Explorer web tool, a publicly available interface where results of the time-limited model are presented and available for research purposes. Users can click on a map and compare what the model predicted from 2013 to 2018 versus what was observed and determine whether the tool actually identified the counties with the highest overdose across the country, including those experiencing new spikes.
“Many of the counties with the most deaths were concentrated in the Midwest and Northeast, where the fentanyl epidemic has hit hardest, but an increasing number of states in the West are affected as well. There’s this idea that this epidemic has been focused in rural areas where the prescription opioid epidemic started, but the reality is overdose deaths have been increasing in cities too. For example, San Francisco and San Diego have seen steep increases in fentanyl overdose deaths in the past year,” Borquez added.
Borquez and Marks note that that all predictive models are limited by the data sets used to inform them and said more timely and available information related to deaths, drug markets and seizures and prescription data at both county and state levels, is urgently needed.
“While our approach can be effective, it also requires that fatal overdose data from all the counties in the U.S. be accessible and available for the current year, which unfortunately is not yet standard practice,” said Borquez. “Our model will only be useful in predicting and preventing deaths if there is no lag in getting data from local and national agencies.”
“Further model refinement and securing access to restricted data through broad collaborations will be next steps to improve model performance. Imagine if we could develop predictive tools for substance use epidemics, similar to what was developed to predict COVID-19 infections and deaths.”
Borquez predicted it would be one to two years before the tool is sufficiently refined to make real-time predictions at a national level based on available data, but that a promising avenue in the short term will involve applying it in states that share recent overdose death information.
“We urgently need methods to predict where these overdoses and other outbreaks may occur. Outbreaks such as hepatitis and HIV are also connected to drug use, and can be prevented too,” said Borquez. “Investing in drug use surveillance and harm-reduction infrastructure doesn’t solve one problem, it solves multiple problems at once.”
Co-authors included: Daniela Abramovitz, Gabriel Carrasco-Escobar, Rocío Carrasco-Hernández, Natasha Martin, Steffanie Strathdee, and Davey Smith from UC San Diego; Christl A Donnelly from University of Oxford, Daniel Ciccarone from UCSF, and Arturo González-Izquierdo from University College London.
Funding was provided by the National Institute on Drug Abuse Avenir grant (DP2DA049295).