The development of drugs to treat cognitive problems in patients with mental illness may be a step closer after a team of researchers discovered that an existing drug – used to treat constipation – may be able to boost our ability to think more clearly.
Severe psychiatric disorders can have a devastating impact on a patient’s life. Cognitive impairments – ranging from decreased attention and working memory to disrupted social cognition and language – are widespread in psychiatric disorders such as major depression, schizophrenia, and bipolar disorder. These common problems are poorly treated with current medications and often have a large impact on people’s lives, and so scientists are searching for ways of improving or restoring these functions.
Previous animal studies have shown that the drugs which target one of the serotonin receptors (the 5-HT4 receptor) have shown promise in improving cognitive function (serotonin is the neurotransmitter which is targeted by SSRI antidepressants). However, it has been difficult to translate these animal findings into humans because of worries about side effects. Now a group of UK researchers have tested an existing approved drug, prucalopride, which targets the 5-HT4 receptor, and found that it may improve cognition. Prucalopride is primarily prescribed for constipation, and has an acceptable level of side effects if taken under medical supervision.
44 healthy volunteers aged 18-36 participated in the trial. 23 were given prucalopride, and 21 were given a placebo. After 6 days all the volunteers were given an fMRI brain scan. Before entering the MRI scanner, volunteers were shown a series of images of animals and landscapes. They viewed these again plus similar images during the scan. After the scan, volunteers performed a memory test: they were asked to distinguish the images they had seen before and during the scan from a set of completely new images.
Presenting the work at the European College of Neuropsychopharmacology conference in Lisbon (with simultaneous publication, see below), lead researcher, Dr Angharad de Cates of the University of Oxford said, “Participants who had taken prucalopride for 6 days performed much better than those receiving placebo on the memory test; the prucalopride group identified 81% of previously viewed images versus 76% in the placebo group. Statistical tests indicate that this was a fairly large effect – such an obvious cognitive improvement with the drug was a surprise to us”.
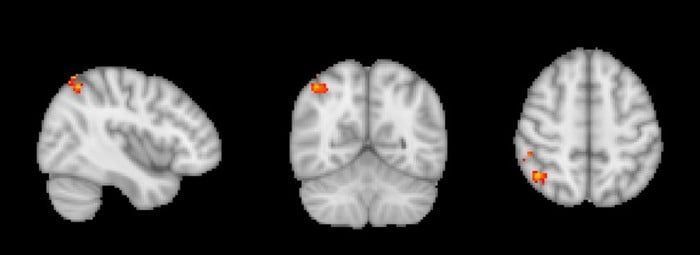
The researchers found that, compared with those taking the placebo, the volunteers taking prucalopride were both significantly better at the memory test after the scan, and also had fMRI scans indicating enhanced activity in brain areas related to cognition. The increased activity was in areas associated with memory, such as the hippocampus (in the centre of the brain) and the right angular gyrus (towards the rear of the brain).
Dr Susannah Murphy (Senior Research Fellow, University of Oxford and a senior author of the study) said, “Even when the low mood associated with depression is well treated with conventional antidepressants, many patients continue to experience problems with their memory. Our study provides exciting early evidence in humans of a new approach that might be a helpful way to treat these residual cognitive symptoms”.
Angharad de Cates said “This is a proof-of-concept study, and so a starting point for further investigation. We are currently planning and undertaking further studies looking at prucalopride and other 5HT4 agonists in patient and clinically vulnerable populations, to see if our findings in healthy volunteers can be replicated and have clinical importance”.
Prucalopride is a 5-HT4 agonist which is taken primarily for constipation. It doesn’t have significant side effects if taken under medical supervision, although doctors caution of the possibility of headache, gastro-intestinal symptoms such as abdominal pain, nausea and diarrhoea, and fatigue or dizziness; there were no significant side-effects shown by any of the volunteers taking prucalopride in this study.
Commenting, Dr Vibe Frokjaer (Adjunct Professor, Dept. Psychology, Copenhagen University) said:
“This study highlights a very interesting and much needed potential for repurposing drugs to help cognitive dysfunction, which is often associated with psychiatric disorders even in remitted states. Importantly, as the authors also state, it will be vital to translate these findings from healthy populations into clinical populations. It will also be important to understand if prucalopride adds to the effects of existing antidepressant treatments, or can be used as a stand-alone therapy”.
To coincide with the ECNP presentation, the work is published today in the peer-reviewed journal Translational Psychiatry (DOI 10.1038/s41398-021-01568-4). The paper is available on request form the ECNP press officer.
This work is presented at the 34th ECNP Annual conference, which takes place in Lisbon and online from 2-5 October, see https://www.ecnp.eu/Congress2021/ECNPcongress . The European College of Neuropsychopharmacology is Europe’s main organisation working in applied neuroscience.
The ECNP thanks Translational Psychiatry for the use of the image. https://www.nature.com/tp/