Findings published this week reveal new insights into the role of fat cells in cognitive decline and neurodegeneration, according to a study that involves the oxidant amplification loop led by Marshall University scientists.
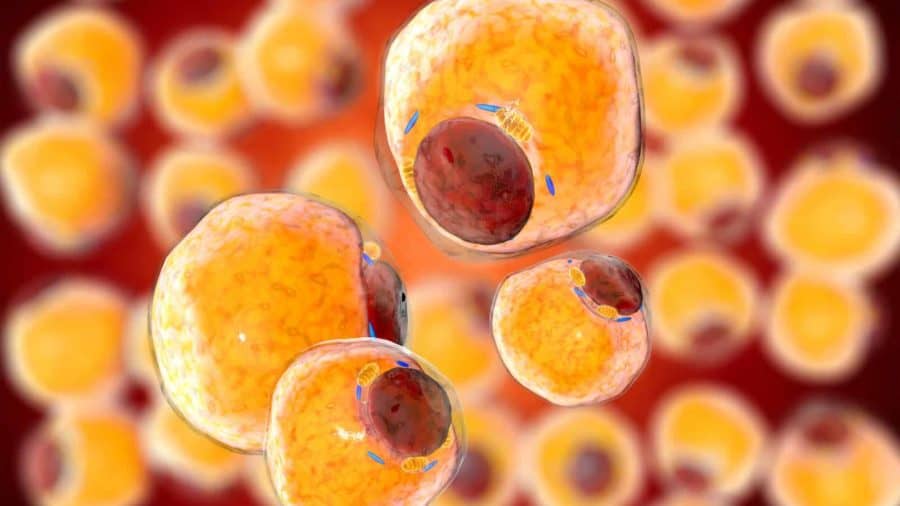
The research, published in iScience, shows that fat cells control the systemic response to brain function, causing impairment in memory and cognition in mice. The activation of Na,K-ATPase oxidant amplification loop affects the expression of important protein markers in fat cells as well as in the hippocampus, which can worsen brain function and lead to neurodegeneration. Targeting the fat cells to antagonize Na,K-ATPase may improve these outcomes.
“We have aimed to demonstrate that Na,K-ATPase signaling, specifically in adipocytes, play a central role in inducing alterations in specific regions of the brain, most notably in the hippocampus, which is critical to memory and cognitive function,” said senior author Joseph I Shapiro, M.D., professor and dean of the Marshall University Joan C. Edwards School of Medicine.
Researchers used a genetically-modified mouse model that released the peptide NaKtide specifically in adipocytes, or fat cells, to find that NaKtide inhibited the signaling function of Na,K-ATPase. The adipocyte-specific NaKtide expression improved the altered phenotype of adipocytes and improved function of the hippocampus, the part of the brain associated with memory and cognition. Inducing oxidative stress through western diet increased production of inflammatory cytokines confined to adipocytes as well as altered protein markers of memory and cognition in the hippocampus.
“Western diet induces oxidant stress and adipocyte alteration through Na,K-ATPase signaling which causes systemic inflammation and affects behavioral and brain biochemical changes,” said Komal Sodhi, M.D., first author and associate professor of surgery and biomedical sciences at the Joan C. Edwards School of Medicine. “Our study showed that adipocyte-specific NaKtide expression in our murine model ameliorated these changes and improved neurodegenerative phenotype.”
This work builds on the groundbreaking work of the late Zijian Xie, Ph.D., who served as director of the Marshall Institute for Interdisciplinary Research from 2013 to 2020. Continued research will help determine if these findings can be confirmed in humans, representing a novel and successful therapeutic target in neurodegenerative disorders. In addition to Shapiro and Sodhi, authors of the paper included Rebecca Pratt, Xiaoliang Wang, Hari Vishal Lakhani, Sneha S. Pillai, Mishghan Zehra, Jiayan Wang, Lawrence Grover, Brandon Henderson, James Denvir, Jiang Liu, Sandrine Pierre and Thomas Nelson, all of Marshall University.
This research was supported by the National Institutes of Health Grants 1R15HL150721 (to K.S.), NIH Bench-to-Bedside award made possible by the Office of Research on Women’s Health (ORWH) 736214 (to K.S. and J.I.S.), and by the BrickStreet Foundation (to J.I.S.) and by the Huntington Foundation, Inc. (J.I.S.). The GABC is supported by WV-INBRE (NIH/NIGMS P20GM103434), the COBRE ACCORD (1P20GM121299), and the WV-CTSI (2U54GM104942).