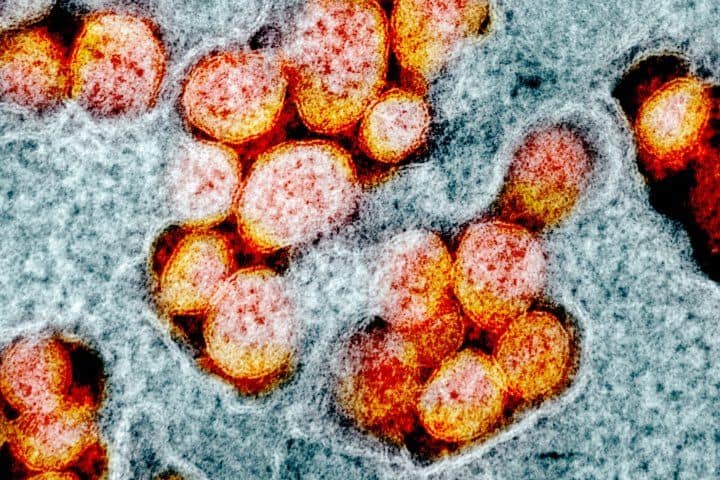
The Alpha variant of SARS-CoV-2 – the first variant of concern – evolved mutations that allowed it to more efficiently suppress the immune system’s early response to infection, according to a new study led by scientists at the UC San Francisco’s Quantitative Biosciences Institute (QBI) and University College London.
The researchers have discovered that the variant has ramped up production of a protein that it uses to stifle infected cells’ immune-stimulating signals. The mutations responsible for this change likely help the Alpha variant evade immune detection and accelerates its transmission, and importantly similar mutations exist in Omicron. The findings are reported in the Dec. 23 issue of Nature.
The team, led by senior authors Nevan Krogan, PhD, of UCSF and Claire Jolly and Greg Towers, PhD, of University College, London, found that Alpha’s enhanced infectivity arose from mutations outside of “spike,” the proteins that have attracted much of scientists’ attention since the start of the pandemic. Spike, which the virus uses to enter the cells of its host, is critical to infection and is the target of all available COVID-19 vaccines. But it is just one of many tools that the virus uses to manipulate its host.
While scientists have closely monitored mutations in the spike region of new variants – Omicron has over 30 – Krogan emphasized that changes in other regions might also have important impact.
“The mutations in spike allow the virus to get into cells more effectively. But what about after the virus gets into cells? There may be other mutations that allow it to replicate more,” said Krogan, who also leads UCSF’s QBI and its Coronavirus Research Group (QCRG).
After it was first detected in the United Kingdom in late 2020, Alpha spread rapidly around the world, suggesting it was significantly more transmissible than the original virus.
But experiments in Towers’ lab indicated that the new variant replicated no faster than its predecessor. Seeking an explanation, the QCRG set out to learn if the new variant interacted differently with the cells it infected.
Studying the variants of concern gives us ideas about how SARS-CoV-2 evolves. Now we have a sense of the proteins that are mutating most frequently, and the biological consequences of those mutations.
The team, which also included researchers at the Massachusetts Institute of Technology (MIT), European Molecular Biology Laboratory (EMBL) and the Icahn School of Medicine at Mount Sinai, compared the variant’s impact on host cells to that of virus isolated early in the pandemic.
To do so, postdoctoral scholar Mehdi Bouhaddou, PhD, QBI senior scientist Lorena Zuliani-Alvarez, PhD, both co-lead authors on the study, measured the activity of each gene and monitored protein levels in lab-grown cells infected by the virus. They also surveyed the phosphorylation status of the proteins – an analysis that detects chemical modifications that can temporarily adjust proteins’ function.
Using this data to compare the response to infection with Alpha and the original virus, the researchers found that many of the significant differences involved the innate immune response, the body’s first line of defense against pathogens. Many of the genes involved in rallying this defense were barely activated in the presence of the SARS-CoV-2 Alpha variant.
In addition, the team discovered that the Alpha-infected cells contained large amounts of three viral proteins known to help the virus evade the body’s immune response. Further experiments showed that one of them, called Orf9b, accomplishes that task by latching on to a protein that switches on immune-stimulating genes.
The findings suggest it may be possible to help the immune system fight SARS-CoV-2 by developing drugs that block this interaction and offer a potential strategy for doing so.
Alpha has since been outpaced by newer variants whose mutations spur even more aggressive transmission. “The virus will keep evolving and adapting to the host, and every time it will adapt better and better,” Zuliani-Alvarez said.
Both the Delta and Omicron appear to be cousins of Alpha, each having mutations in two of the three regions the team studied, suggesting they may have similar effects on the innate immune system.
The findings demonstrate the value of understanding the full scope of changes shaping the behavior of viral variants. “Studying the variants of concern gives us ideas about how SARS-CoV-2 evolves,” said Bouhaddou. “Now we have a sense of the proteins that are mutating most frequently, and the biological consequences of those mutations. I think this helps us prepare for what might come next.”
The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF’s primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area.
About QBI: The Quantitative Biosciences Institute (QBI) fosters collaborations across the biomedical and the physical sciences, seeking quantitative methods to address pressing problems in biology and biomedicine. Motivated by problems of human disease, QBI is committed to investigating fundamental biological mechanisms, because ultimately solutions to many diseases have been revealed by unexpected discoveries in the basic sciences. Learn more at qbi.ucsf.edu.