Confronted by dangerous and challenging diseases such as the COVID-19 pandemic, scientists strive to understand the interactions between virus and human cells with hopes that the knowledge will lead to means to prevent, treat and cure the condition. With this idea in mind, the lab of Dr. Pedro Piedra at Baylor College of Medicine and his colleagues have developed a miniature model of the human nose that enabled them study the complex interactions between human cells and two important viruses and to test the efficacy of therapies.
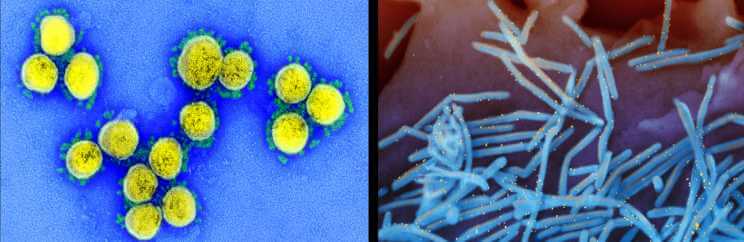
The team studied SARS-CoV-2, the virus that causes COVID-19, and the respiratory syncytial virus (RSV), a major pediatric respiratory virus.
“In the case of these respiratory viruses, the infection begins in the nose when one breathes in the virus,” said Piedra, professor of molecular virology and microbiology, pediatrics and of pharmacology and chemical biology at Baylor and corresponding author of the work. He also is the director of Baylor’s Clinical Laboratory Improvement Amendments (CLIA)-Certified Respiratory Virus Diagnostic Laboratory. “To study virus-human cell interactions, we have developed a versatile human nose organoid – a laboratory representation of the cells layering the inside of the nose where the first events of a natural viral infection take place.”
Human nose organoids provide access to the inside of the human nose, enabling researchers to study the early events of the infection in the lab, something they had not had before. They have successfully developed human nose organoids from both adults and infants.
A miniature human nose model
The cells lining the inside of the nose, the epithelium, are exposed to air on one side and to the blood circulatory system on their opposite side.
“Our three-dimensional organoid system replicates this natural situation in the lab using nose epithelium harvested with a nasal swab,” explained first author Dr. Anubama Rajan, postdoctoral associate in the Piedra lab. “We grow the harvested epithelium in tissue culture plates that provide an air-liquid interphase, where the top side of the epithelium is exposed to air and the bottom side is bathed in liquid that provides nutrients and other factors.”
To study the interaction between SARS-CoV-2 or RSV and the nose epithelium, the researchers simulated a natural infection by placing each virus separately on the air side of the culture plates and studying the changes that occurred on the nose organoid.
“We observed divergent responses to SARS-CoV-2 and RSV infection,” said co-author Dr. Vasanthi Avadhanula, assistant professor of molecular virology and microbiology at Baylor . “SARS-CoV-2 induces severe damage to the epithelium, no interferon response (an antiviral first defense response), and minimal mucus secretion. In striking contrast, RSV induces abundant mucus secretion and a profound interferon response.”
Testing therapies
The team also used their human nose organoid model of RSV infection to test the efficacy of palivizumab, an FDA-approved monoclonal antibody to prevent severe RSV disease in high-risk infants. In this case, they placed the therapeutic monoclonal antibody in the liquid-filled chamber to more closely resemble the human experience where therapeutic antibodies enter the blood circulation and provide protection of the airways against RSV infection.
“In our model, palivizumab effectively prevented RSV infection in a concentration-dependent manner,” said Avadhanula, co-director of the (CLIA)-Certified Respiratory Virus Diagnostic Laboratory and of the lab’s research program.
Previous models were produced using invasive lung or nose biopsy or broncho alveolar lavage.
Another advantage of using this novel human nose organoid system is that it can reveal how a person’s initial control of the infection occurs and provide insights into what would make a person more susceptible to a virus than another. Researchers also can use this system to study other respiratory viruses and potentially other disease-causing microbes.
Learn all the details of this work in the journal mBIO.
Other contributors to this work include Ashley Morgan Weaver, Gina Marie Aloisio, Joseph Jelinski, Hannah L. Johnson, Susan F. Venable, Trevor McBride, Letisha Aideyan, Felipe-Andrés Piedra, Xunyan Ye, Ernestina Melicoff-Portillo, Malli Rama Kanthi Yerramilli, Xi-Lei Zeng, Michael A. Mancini, Fabio Stossi, Anthony W. Maresso, Shalaka A. Kotkar, Mary K. Estes and Sarah Blutt, all at Baylor College of Medicine.
This work was supported by Public Health Service grant P30DK056338, NIH grants (DK56338, CA125123, ES030285, T32AI055413, U19 AI144297 and U19 Al116497), Cancer Prevention and Research Institute of Texas (CPRIT; RP150578, RP170719), the Dan L. Duncan Comprehensive Cancer Center and the John S. Dunn Gulf Coast Consortium for Chemical Genomics.