Prostate cancer can come back from common hormone deprivation therapy with a vengeance and no clear treatment option, but scientists have early evidence that one way to kill these recurring cancer cells may be with a lot of iron.
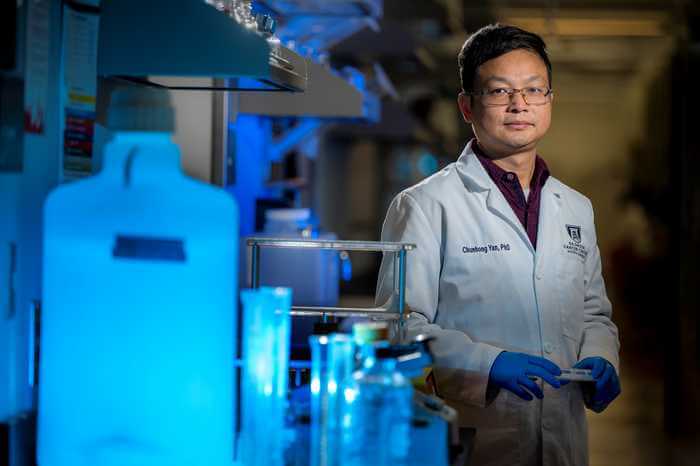
The metal that is key to our red blood cells carrying oxygen and other body fundamentals also is known to be lethal to cells in big doses, but prostate cancer cells are essentially impervious to it, says Dr. Chunhong Yan, molecular biologist at the Georgia Cancer Center and Department of Biochemistry and Molecular Biology at the Medical College of Georgia.
Yan is putting together a strategy to change that and enable death by iron for treatment resistant prostate cancer through a process called ferroptosis. Despite its essentiality, at high levels, iron generates also high levels of toxic free radicals, or ROS, whose consequences include damaging lipids, or fats, that also are essential to cell function.
“When the cell takes up iron, it goes through different processes, which generate a lot of ROS,” says Yan, principal investigator on a new $1.1 million idea development award from the U.S. Department of Defense.
While it’s usual for iron and ROS to interact, when levels of both are high it damages lipids, an important component of cell membranes.
“What we are trying to do is to take advantage of this side effect to treat prostate cancer,” Yan says.
Through this process called lipid peroxidation, lipids, which also are important energy stores for cells and for internal cell signaling, aggregate, lose their flexibility and their efficiency and ultimately the cell dies, although exactly why remains a bit of a mystery.
Those lipid changes sound and are very destructive, but prostate cancer can be particularly insensitive to them and to drugs designed to induce this sort of excess iron damage, because the cancer cells already require some similar changes to lipids in the cell membrane to ensure they have the large amount of energy they need to survive, grow and spread.
But the MCG research team has found that the gene, ATF3, a regulator of cell stress which they have shown also can suppress prostate cancer, can make prostate cancer cells more vulnerable to a newer compound, JKE-1674, that can help induce ferroptosis.
Basically, if you reduce prostate cancer cells’ ability to ignore stress, they will die, Yan says.
Another piece of the puzzle they have found is that the drug bortezomib, a chemotherapy agent used to treat multiple myeloma, a cancer of the plasma cells that normally produce antibodies to help protect us from infections, is a good partner because it can increase expression of ATF3, or activating transcription factor 3. ATF3 in turn induces expression of HMOX1, an enzyme and known antioxidant which basically cuts iron loose from places like hemoglobin so more can accumulate inside cells, which is lethal.
One more piece is the body’s natural mechanism to cope with this unhealthy pairing of iron and ROS so that a lot of good cells don’t die as a result. It’s called glutathione peroxidase 4, or GPX4, an antioxidant and inhibitor of ferroptosis. One way JKE-1674 works is by inhibiting GPX4, which has the added advantage of repairing some of the damage to the lipids that makes prostate cancer cells insensitive to death by ferroptosis. These kinds of inhibitors have already shown promise in cancer treatment, Yan says.
Yan notes that clinical trials indicated bortezomib is not particularly effective at treating prostate cancer, but in combination with JKE-1674, they have laboratory evidence it becomes a powerful foe against the common cancer.
In a cell culture, Yan’s team has watched increased ATF3 expression sensitize human prostate cancer cells to death by iron, and the new DOD funded studies are enabling the next steps: studying the induction in a mouse with human prostate cancer, called a humanized mouse model, to see whether ATF3-induced bortezomib paired with JKE-1674 again induces ferroptosis in advanced, typically lethal prostate cancer.
They also have a new genetically engineered mouse that also generates more ATF3 and will see whether that makes prostate cancer more vulnerable to ferroptosis as well.
Yan and his colleagues also want to learn more about how ATF3 makes prostate cancer cells more vulnerable to death by iron with the help of agents like bortezomib.
Yan’s lab is taking advantage of existing drugs and drug regimens to efficiently identify a therapy that could comparatively quickly go from his lab to a clinical trial for the most common cancer in American men, other than nonmelanoma skin cancer, and second leading cause of cancer death, behind lung cancer, according to the American Cancer Society.
As an example, patients get an injection of bortezomib for multiple myeloma, and Yan is sticking to that schedule for his studies to try to ensure translatability of the lab work into people and so, if they continue to find success, rapid movement to a clinical trial.
There are currently a variety of treatments for hormone, androgen-driven prostate cancer, and many therapies are geared at reducing levels of the male hormones, like testosterone, and/or stopping them from directly fueling prostate cancer, including surgical castration to remove the testicles, which produce most of the androgens, and giving drugs that bind to the androgen receptors so the hormones can’t be active.
While these therapies are typically effective initially, some cancers become treatment resistant typically in 18-24 months, Yan says, which dramatically limits available options, including a significant number of prostate cancers that become resistant to even newer generation drugs, like the hormone therapy enzalutamide.
“That is why it’s very important to find some therapy to treat this group of patients,” Yan says.
Ferroptosis was first described as a distinct form of cell death in 2012.