Have a cough, sore throat and congestion? Any number of respiratory viruses could be responsible.
Conventional tests can identify certain likely culprits by relying on chemical reactions, but some researchers want to swap chemistry for electrical changes sensed by nanomaterials. Today, scientists report using a single-atom-thick nanomaterial to build a device that can simultaneously detect the presence of the viruses that cause COVID-19 and the flu — at much lower levels and much more quickly than conventional tests for either.
The researchers will present their results at the spring meeting of the American Chemical Society (ACS). ACS Spring 2023 is a hybrid meeting being held virtually and in-person March 26–30, and features more than 10,000 presentations on a wide range of science topics.
The symptoms of both flu and COVID-19 overlap considerably, making it difficult to distinguish between them, notes Deji Akinwande, Ph.D., who is presenting the work at the meeting.
“When both of these viruses are circulating together as they did earlier this winter, it would be immensely useful to have a sensor that can simultaneously detect whether you have COVID, flu, none of the above or both,” he says.
Akinwande, who is at The University of Texas at Austin, says that the device he and colleagues are developing could be modified to test for other infections as well.
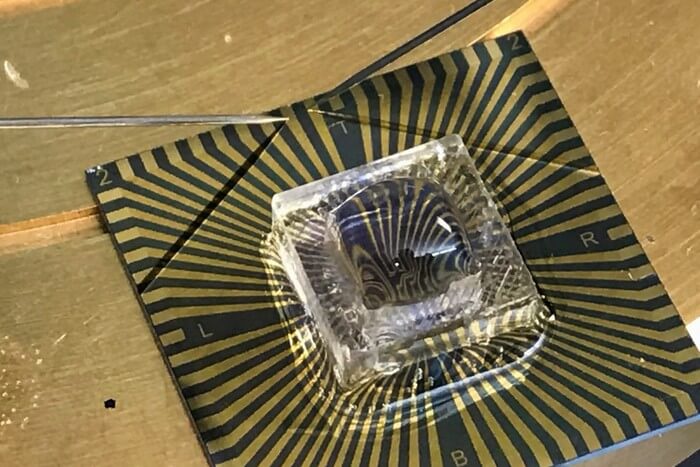
The group, including Dmitry Kireev, Ph.D., a postdoc in Akinwande’s lab, constructed the COVID-19 and flu sensor using graphene, a single layer of carbon atoms arranged in a hexagonal lattice pattern. Its extreme thinness renders graphene highly sensitive to any electrical changes in its environment. Akinwande and other researchers see enormous potential in using it and other, similar nanomaterials to create sensors for many different applications.
“These ultra-thin nanomaterials generally hold the record for best sensitivity, even down to the detection of single atoms, and they can improve the ability to detect very small quantities of basically anything that needs to be sensed, whether it’s bacteria or viruses, in gas or in blood,” Akinwande says.
Previously, his group reported designing a graphene-based temporary tattoo that could monitor blood pressure. The tattoo consists of pairs of sensors placed along the arteries of the arm. One half of each pair sends out an electrical current that its partner detects. This signal is used to determine blood flow.
To build the infection sensor, the researchers had to make graphene respond to the presence of viral protein. To do so, they looked to the immune system, which produces antibodies that are fine-tuned to recognize and latch onto particular pathogens. The researchers linked antibodies against SARS-CoV-2, the virus that causes COVID-19, and against the flu virus to graphene. When a sample from an infected person is placed on the sensor, these antibodies bind to their target proteins, prompting a change in the electrical current.
The researchers did not have the safety facilities needed to use whole, active flu or SARS-CoV-2 viruses to test the roughly square-inch sensor. To substitute, they used proteins from these viruses delivered in fluid intended to resemble saliva. Their results indicated that not only could the sensor detect the presence of the proteins, it could do so when they were present at extremely low quantities. This sensitivity suggested the sensor could be used for detecting the much more sparse viral particles found in breath, Akinwande says.
The sensor also worked quickly, returning results within about 10 seconds of dropping in a sample, he says. By comparison, conventional COVID-19 tests can take minutes or hours, depending on the type, and a dual COVID and flu test recently authorized by the U.S. Food and Drug Administration takes about half an hour to produce results.
Akinwande and his group are working to improve its performance further, including by expanding the slate of viruses it can detect. With funding from the National Science Foundation, they are developing a sensor designed to test for SARS-CoV-2 variants, such as omicron and delta. While they are currently focusing on a two-variant design, the test could be adapted to simultaneously identify even more, they say.