In the ongoing search for a cure for Alzheimer’s disease, a burgeoning branch of medicine is bringing new hope. Stem cell therapies are already being used to treat various cancers and disorders of the blood and immune system. In a new proof-of-concept study, scientists at University of California San Diego show stem cell transplants may also be a promising therapeutic against Alzheimer’s.
In the study, publishing this month in Cell Reports, the researchers demonstrate that transplanting hematopoietic stem and progenitor cells was effective in rescuing multiple signs and symptoms of Alzheimer’s in a mouse model of the disease. Mice that received healthy hematopoietic stem cells showed preserved memory and cognition, reduced neuroinflammation and significantly less β-amyloid build-up compared to other Alzheimer’s mice.
“Alzheimer’s is a very complex disease, so any potential treatment has to be able to target multiple biological pathways,” said senior study author Stephanie Cherqui, PhD, professor at UC San Diego School of Medicine. “Our work shows that hematopoietic stem and progenitor cell transplantation has the potential to prevent complications from Alzheimer’s and could be a promising therapeutic avenue for this disease.”
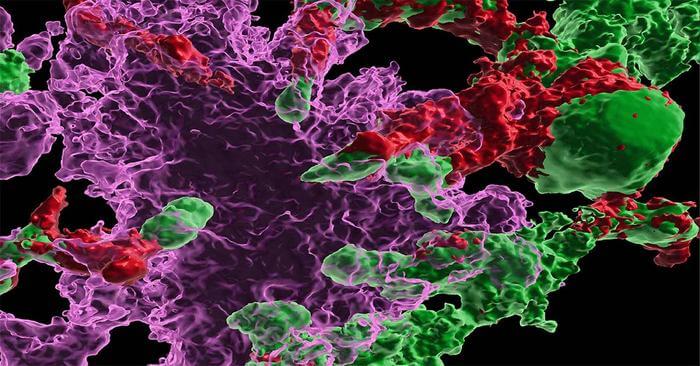
The success of the therapy stems from its effects on microglia, a type of immune cell in the brain. Microglia have been implicated in the initiation and progression of Alzheimer’s disease in various ways. It’s known that sustained microglia inflammation can contribute to Alzheimer’s, as the release of inflammatory cytokines, chemokines and complement proteins leads to increased β-amyloid production. In healthy conditions, microglia also play a major role in clearing β-amyloid plaques, but this function is impaired in Alzheimer’s. The resulting β-amyloid build-up also puts stress on other brain cells, including endothelial cells that affect blood flow to the brain.
Postdoctoral researcher and first author Priyanka Mishra, PhD, set out to test whether transplanting stem cells could lead to the generation of new, healthy microglia that might reduce the progression of Alzheimer’s disease. The Cherqui lab had already found success using similar stem cell transplants to treat mouse models of cystinosis, a lysosomal storage disease, and Friedreich’s ataxia, a neurodegenerative disease.
Mishra and her colleagues performed systemic transplantations of healthy wild-type hematopoietic stem and progenitor cells into Alzheimer’s mice and found that the transplanted cells did differentiate into microglia-like cells in the brain.
The researchers then evaluated the animals’ behavior and found that memory loss and neurocognitive impairment were completely prevented in mice that received the stem cell transplant. These mice showed better object recognition and risk perception, as well as normal anxiety levels and locomotor activity, compared to non-treated Alzheimer’s mice.
Looking closer at the animals’ brains, the researchers found that mice treated with healthy stem cells showed a significant reduction in β-amyloid plaques in their hippocampus and cortex. The transplant also led to reduced microgliosis and neuroinflammation, and helped preserve the integrity of the blood-brain barrier.
Finally, the researchers used transcriptomic analyses to measure the expression of different genes in treated and non-treated Alzheimer’s mice. Those that had received the stem cell therapy had less cortical expression of genes associated with diseased microglia, and less hippocampal expression of genes associated with diseased endothelial cells.
Altogether, the transplantation of healthy hematopoietic stem and progenitor cells led to enhanced microglia health, which in turn protected against multiple levels of Alzheimer’s pathology.
Importantly, a third group of mice that received stem cells isolated from Alzheimer’s mice exhibited no signs of improvement, demonstrating that these cells retained the disease-related information in Alzheimer’s disease.
Future studies will further explore how the healthy transplanted cells produced such significant improvements, and whether similar transplant strategies can be used to alleviate Alzheimer’s symptoms in humans.
“Alzheimer’s disease poses a major emotional and economic burden on our society, yet there is no effective treatment available,” said Cherqui. “We are excited to see such promising preclinical results from hematopoietic stem cell therapy and look forward to developing a new therapeutic approach for this devastating disease.”
Co-authors of the study include: Alexander Silva, Jay Sharma, Jacqueline Nguyen, Donald P. Pizzo and Debashis Sahoo, all at UC San Diego, as well as Denise Hinz at the La Jolla Institute for Immunology.