Analysis of data from more than 1 million Danish inpatients identifies nearly 4,000 drug pairings that are associated with more frequent dosage adjustments when prescribed together—potentially hinting at previously undiscovered drug interactions. Søren Brunak of the University of Copenhagen, Denmark, and colleagues present these findings in the open-access journal PLOS Digital Health.
In some cases, especially among elderly populations, a person may be prescribed several different medications at once in order to treat one or multiple health conditions—a phenomenon known as polypharmacy. Polypharmacy is associated with increased health risks due to the potential for harmful interactions between different drugs. Polypharmacy research has typically focused on the number and type of drugs a patient receives. However, the dosage of each drug may also influence interactions and health outcomes.
To deepen understanding of polypharmacy in the context of drug dosage, Leal, Haue, Brunak and colleagues analyzed data from the electronic health records of more than 1 million patients admitted as inpatients in Danish hospitals from 2008 to 2016. They used a statistical approach known as Bayesian inference to identify drug pairings associated with more frequent adjustments to the dosage of the drugs.
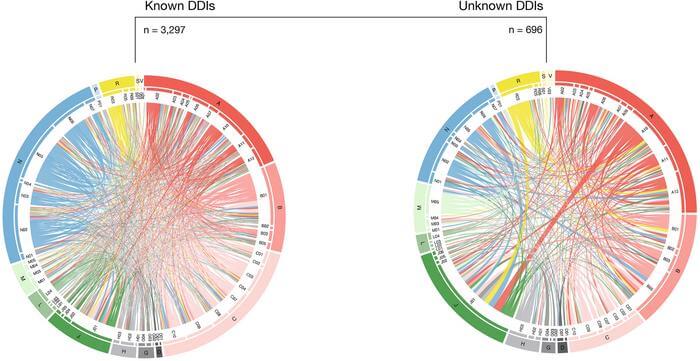
Out of 77,249 total drug pairings, 3,993 were associated with more frequent dosage adjustments when given together. Further analysis showed that, of the pairs associated with more frequent dosage adjustments, 2,412 were also associated with hospital readmission, mortality, or longer hospital stays, and 308 were associated with worsened kidney function.
Many of the drug pairs associated with dosage adjustments have already been linked by previous research to potential harmful drug interactions. However, 694 have not, and while this study does not prove any cause-effect relationships, the authors suggest that some of these drug pairings may involve previously undiscovered interactions. These are often given to fewer patients and therefore harder to detect in small scale studies – contrary to the 185 million treatment episodes used in this study. Future research will be needed to explore that possibility.
Overall, these findings help deepen understanding of links between drug dosage and polypharmacy, and could help guide future evaluation of drug interactions and efforts to reduce the risks of polypharmacy for patients.