For the first time, a research team at The Hospital for Sick Children (SickKids) has uncovered a way to potentially reduce the amount of toxic cellular waste accumulating in patients with Zellweger Spectrum Disorder (ZSD).
ZSD is a group of rare, neurodegenerative genetic conditions caused by genetic variations that reduce the number of peroxisomes – the parts of cells that are responsible for, among other tasks, breaking down fats. ZSD varies in severity and is characterized by progressive neurodegeneration as well as symptoms that range from visual impairments, such as cataracts, to liver and kidney disfunction.
Like all living things, cellular structures break down over time and must be recycled. In cells, this recycling process is called autophagy. Autophagy in people with ZSD is affected by the lack of working peroxisomes that ultimately causes damage to other parts of the cell, resulting in a buildup of toxic cellular waste that can be fatal. Until now, the connection between peroxisome loss and the disruption in the recycling process in ZSD was unknown.
In a study published in Nature Communications, researchers led by Dr. Peter Kim, a Senior Scientist in the Cell Biology program at SickKids, and Dr. Robert Bandsma, a Scientist in the Translational Medicine program, discovered that by genetically and pharmaceutically increasing a cell’s ability to recycle its own components it is possible to clear damaged cellular material, providing a new therapeutic target for treating ZSD.
Looking closely at cellular recycling
There are more than a dozen known pathways that recycle specific damaged or irrelevant components in a cell. One of these pathways is pexophagy which selectively recycles peroxisomes.
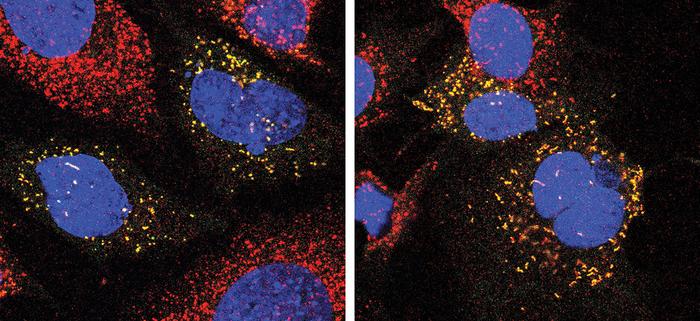
Previous research from the Kim-Bandsma team found that the most common genetic variation that causes ZSD significantly increases pexophagy, causing healthy peroxisomes to get recycled alongside unhealthy ones. In the new study, Dr. Kyla Germain, a former graduate student in Kim and Bandsma’s labs, found that this increase in pexophagy can also prevent cells from degrading other cellular waste.
“Our work demonstrates for the first time that different cellular recycling pathways can influence one another,” Germain explains. “A cell’s recycling system has a maximum load capacity – an autophagic limit. When this limit is exceeded, toxic cellular waste will accumulate.”
After locating this connection between different recycling pathways, researchers found they could optimize the overall recycling process by increasing the autophagic limit. In doing so, they observed improved clearance of cellular waste, which opens new pathways to treat ZSD.
“These results are exciting as they show that through understanding a fundamental process that takes place in all our cells, we can potentially develop new and better treatments for a very serious condition,” says Bandsma, who is also a Staff Physician in the Division of Gastroenterology, Hepatology and Nutrition at SickKids.
Informing care beyond ZSD
The research team is hopeful that findings from this study may inform research in other neurodegenerative conditions that are associated with changes in autophagy, such as Huntington’s disease and Parkinson’s disease.
“We identified that protein aggregates involved in Huntington’s disease and Parkinson’s disease can also prevent the turnover of damaged peroxisomes, which means scientists may be able to target these components in patients outside the field of ZSD,” Kim says.
The Kim-Bandsma team’s next step is to take this research into a pre-clinical ZSD models to test various therapeutics that could either increase autophagy or inhibit pexophagy. These studies will be done using the expertise at the SPARC Drug Discovery core facility at SickKids.
This work was supported by the Canada Institutes of Health Research (CIHR), the Ontario Graduate Scholarship, a Hayden Hantho Award and the Hilda and William Courtney Clayton Paediatric Research Fund.