For the roughly 1.5 million Americans who survive a traumatic brain injury each year, health outcomes can vary widely. These injuries can lead to a range of problems, from loss of coordination and depression to an increased risk of developing dementia in the future. A team of scientists at Gladstone Institutes has now uncovered, on a molecular level, how traumatic brain injuries trigger neurodegeneration and how to target that process to prevent long-term damage.
Blood Protein Fibrin Plays a Causative Role in Brain Damage
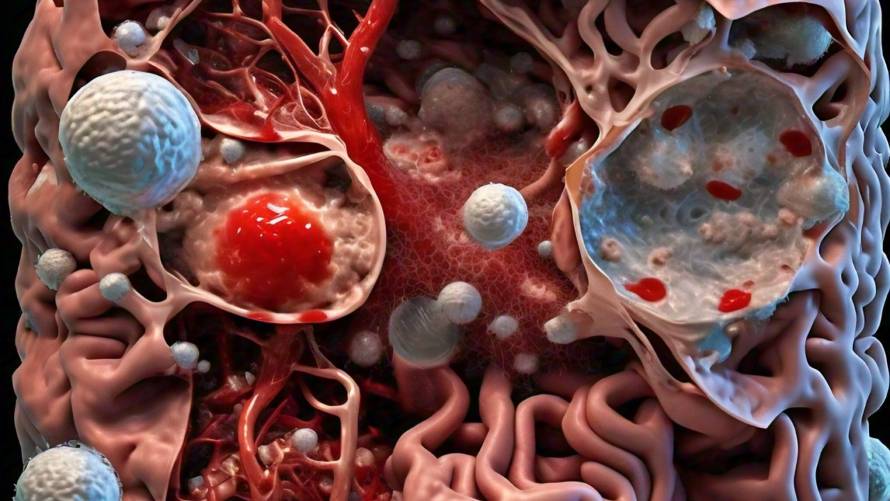
The study, led by Jae Kyu Ryu, PhD, a scientific program leader in the lab of Katerina Akassoglou, PhD at Gladstone Institutes, focused on the role of a specific blood protein called fibrin. While it was known that fibrin was present in the brain after traumatic brain injury, the researchers discovered that it plays a causative role in brain damage.
“Across many neurological diseases, toxic immune responses in the brain are triggered by blood leaks and drive neurodegeneration,” says Akassoglou, a senior investigator at Gladstone and the director of the Center for Neurovascular Brain Immunology at Gladstone and UCSF. “Neutralizing the toxic immune responses in the brain paves the way to new therapies for neurological diseases.”
Fibrin Turns Good Immune Cells Bad, Causing Inflammation and Neuron Death
Using state-of-the-art imaging technology, the Gladstone team studied mouse and human brains, revealing that fibrin is responsible for turning good immune cells bad, causing dangerous inflammation and unleashing toxins that kill neurons. The researchers leveraged genetic tools with a specific mutation in fibrin that can block it from activating immune cells without affecting its beneficial blood-clotting abilities.
Akassoglou’s lab had previously developed a drug, a therapeutic monoclonal antibody, that acts only on fibrin’s inflammatory properties without adverse effects on blood coagulation. This fibrin-targeting immunotherapy protects from multiple sclerosis and Alzheimer’s disease in mice, and a humanized version is already in Phase 1 safety clinical trials by Therini Bio.
“It’s exciting to have a therapeutic option to neutralize blood toxicity in neurologic diseases,” Ryu says. “Future studies are needed to test the effects of the fibrin immunotherapy in traumatic brain injury.”
Implications for Improving Outcomes after Brain Injuries
Lennart Mucke, MD, director of the Gladstone Institute of Neurological Disease, notes that this study identifies a potential new strategy to diminish the devastating impacts of brain injuries. “Brain injuries can have profound effects on a person’s cognitive abilities, emotional health, and motor skills, touching every part of their life,” he says. “It will be interesting to explore whether blocking the disease-promoting effects of fibrin can improve the outcome of brain surgeries and reduce disability when implemented after traumatic brain injuries have occurred.”