A new study funded by the National Institutes of Health (NIH) reveals that a self-adjusting brain implant could significantly improve treatment for Parkinson’s disease symptoms. This adaptive deep brain stimulation (aDBS) device responds to changes in brain activity, potentially offering more personalized and effective care for individuals with Parkinson’s.
Personalized Medicine: How aDBS Works
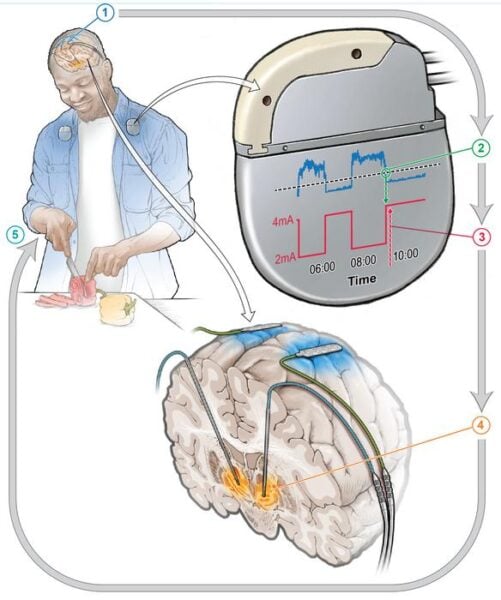
Deep brain stimulation (DBS) has been used for years to treat Parkinson’s disease and other brain disorders. It involves implanting electrodes into specific brain areas to deliver electrical signals that help control symptoms. Traditional DBS provides constant stimulation, which can sometimes lead to unwanted side effects.
The new aDBS system takes a more nuanced approach. It uses machine learning to analyze real-time brain activity data and adjust the level of stimulation as needed throughout the day. This personalized approach aims to provide the right amount of treatment at the right time, potentially reducing side effects and improving overall symptom management.
Dr. Megan Frankowski, a program director for NIH’s BRAIN Initiative, which helped fund the project, explains the significance: “This study marks a big step forward towards developing a DBS system that adapts to what the individual patient needs at a given time. By helping to control residual symptoms while not exacerbating others, adaptive DBS has the potential to improve the quality of life for some people living with Parkinson’s disease.”
Promising Results: aDBS vs. Conventional DBS
The small feasibility study involved four participants who were already receiving conventional DBS treatment. Each participant identified their most bothersome persistent symptom, which was often either involuntary movements or difficulty initiating movement.
The researchers then set up the aDBS system alongside the existing DBS therapy. After several months of training the aDBS algorithm, participants were sent home for a comparison test. The study alternated between conventional DBS and aDBS treatments every two to seven days.
The results were striking:
1. aDBS improved each participant’s most bothersome symptom by approximately 50% compared to conventional DBS.
2. Three out of four participants could often correctly guess when they were receiving aDBS treatment due to noticeable symptom improvement, even though they weren’t told which treatment they were receiving at any given time.
These findings suggest that aDBS could offer significant benefits over conventional DBS for some individuals with Parkinson’s disease.
Why it matters: Parkinson’s disease affects an estimated 1 million people in the United States and 10 million worldwide. As the second most common neurodegenerative disorder after Alzheimer’s disease, improving treatment options for Parkinson’s could have a substantial impact on public health. The development of aDBS represents a step towards more personalized and effective care for individuals living with this challenging condition.
The adaptive nature of this new treatment could also help address some limitations of current therapies. For example, the effectiveness of levodopa, a common Parkinson’s medication, can fluctuate throughout the day as drug levels in the brain rise and fall. aDBS could potentially smooth out these fluctuations by providing increased stimulation when drug levels are high and decreasing stimulation as they drop, offering more consistent symptom relief.
While the results are promising, challenges remain before aDBS can become widely available. The initial setup of the device requires significant input from highly trained clinicians. However, researchers envision a future where most of the work would be managed by the device itself, reducing the need for frequent clinic visits and potentially increasing access to this advanced treatment.
Dr. Frankowski highlights the potential impact on treatment accessibility: “If there were a way for a system to find the most optimal settings at the press of a button, that would really increase the availability of this treatment for more people.”
As research continues, the development of aDBS technology represents an exciting frontier in the treatment of Parkinson’s disease and potentially other neurological disorders. By harnessing the power of machine learning and personalized medicine, this self-adjusting brain pacemaker could offer new hope for improved quality of life for millions of people worldwide.