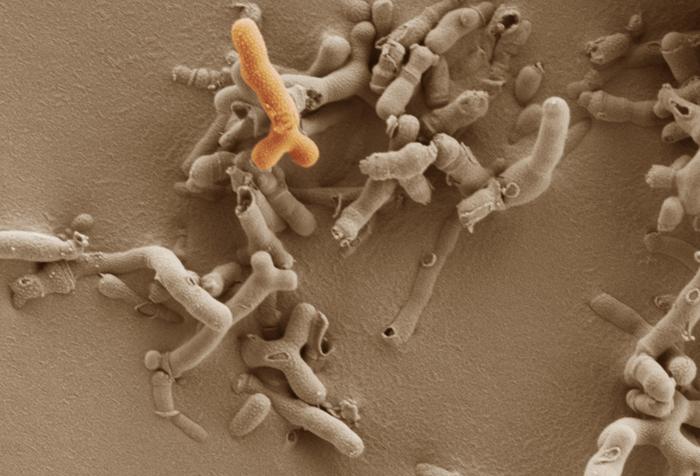
A new study from the University of Cambridge reveals that a common probiotic bacteria found in the maternal gut during pregnancy could play a crucial role in fetal brain development. The research, conducted on mice, suggests that Bifidobacterium breve may enhance nutrient transport to the fetal brain and promote beneficial changes in cell processes related to growth.
The Gut-Brain Connection: From Mother to Child
The study, published in Molecular Metabolism, compared fetal brain development in mice whose mothers had no gut bacteria to those whose mothers were given Bifidobacterium breve orally during pregnancy. The results were striking: fetuses of mothers given the probiotic showed increased nutrient transport to the brain and other positive changes in cell processes linked to growth.
Dr. Jorge Lopez-Tello, the study’s lead author, explains the significance: “Our study suggests that by providing ‘good bacteria’ to the mother we could improve the growth and development of her baby while she’s pregnant.”
Bifidobacterium breve is a naturally occurring beneficial bacteria in the human gut and is commonly available as a supplement in probiotic drinks and tablets. This research opens up new possibilities for supporting fetal development, particularly in cases where maternal health factors might compromise optimal growth.
The potential implications of this research extend beyond immediate fetal growth. Low birth weight and fetal growth restriction are associated with increased risks of various conditions later in life, including cerebral palsy in infants, anxiety, depression, autism, and schizophrenia. By promoting healthier fetal brain development, probiotic interventions during pregnancy could potentially reduce the risk of these long-term health issues.
Rethinking Fetal Growth Interventions
The findings challenge conventional approaches to addressing fetal growth restriction, a condition affecting up to 10% of firstborn babies. Professor Amanda Sferruzzi-Perri, senior author of the study, points out: “The design of therapies for fetal growth restriction are focused on improving blood flow pathways in the mother, but our results suggest we’ve been thinking about this the wrong way – perhaps we should be more focused on improving maternal gut health.”
This shift in perspective could lead to safer, more natural interventions for supporting fetal growth. Dr. Lopez-Tello suggests that “future treatments for fetal growth restriction could potentially focus on altering the gut microbiome through probiotics, rather than offering pharmaceutical treatments – with the risk of side effects – to pregnant women.”
The research is significant for several reasons. It suggests a non-invasive, potentially low-risk method for supporting fetal development. By addressing fetal growth issues early, it could reduce the risk of various health problems throughout life. As we learn more about the maternal microbiome, it may be possible to tailor probiotic interventions to individual needs. Probiotic supplements are generally affordable and widely available, making this a potentially accessible intervention for many pregnant women. It also underscores the interconnectedness of maternal and fetal health, emphasizing the importance of overall well-being during pregnancy.
While the results are promising, it’s important to note that this study was conducted on mice. Professor Lindsay Hall from the University of Birmingham, who was involved in the research, cautions: “Although further research is needed to understand how these effects translate to humans, this exciting discovery may pave the way for future clinical studies that explore the critical role of the maternal microbiome in supporting healthy brain development before birth.”
The researchers plan to continue their work, monitoring brain development in offspring after birth and investigating how Bifidobacterium breve interacts with other gut bacteria in natural settings. This ongoing research could provide valuable insights into the complex relationship between maternal gut health and fetal development.
Why It Matters:
This research opens up new possibilities for supporting fetal health and development through relatively simple interventions. If the findings translate to humans, it could provide a cost-effective, low-risk way to improve outcomes for babies, potentially reducing the incidence of various developmental and neurological issues. Moreover, it highlights the importance of maternal gut health during pregnancy, an area that has received relatively little attention until now. As we face rising rates of obesity and chronic stress, which can negatively impact the maternal gut microbiome, understanding how to support a healthy microbial balance becomes increasingly crucial for both maternal and fetal health.
As we await human trials and further research, expectant mothers should consult with their healthcare providers before making any changes to their diet or supplement regimen. However, this study highlights the potential importance of maintaining a healthy gut microbiome during pregnancy, opening up new avenues for supporting maternal and fetal health.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!