Summary: Researchers at Washington University School of Medicine have developed a novel approach to treat glioblastoma by making cancer cells visible to the immune system. The strategy combines two FDA-approved drugs to force brain cancer cells to display targets that immune cells can attack, potentially opening new avenues for immunotherapy treatment.
Journal: Nature Genetics, September 2, 2024, DOI: 10.1038/s41588-024-01880-x | Reading time: 4 minutes
A New Hope for Brain Cancer Treatment
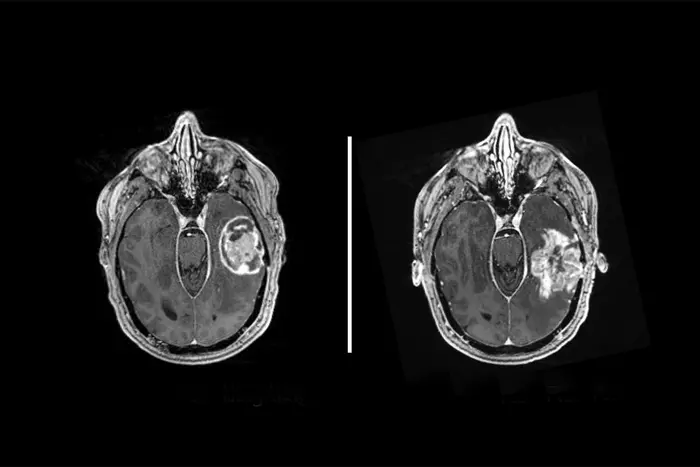
Glioblastoma remains one of medicine’s most formidable challenges, with patients typically surviving less than two years after diagnosis, even with advanced treatments. However, researchers at Washington University School of Medicine in St. Louis have discovered a potential breakthrough: a way to make these elusive cancer cells visible to the body’s immune system.
The research team, led by Dr. Ting Wang and Dr. Albert H. Kim, has demonstrated a method to force glioblastoma cells to display immune system targets using a combination of two existing FDA-approved cancer drugs. “For patients whose tumors do not naturally produce targets for immunotherapy, we showed there is a way to induce their generation,” said Wang, the Sanford C. and Karen P. Loewentheil Distinguished Professor of Medicine and head of the Department of Genetics at WashU Medicine.
Exploiting Cancer’s Hidden Vulnerabilities
The strategy focuses on DNA segments called transposable elements, which can produce unique proteins found only in tumor cells. These proteins, known as tumor antigens or neoantigens, could serve as targets for various immunotherapy approaches, including vaccines and engineered T cell therapies.
The researchers used two epigenetic therapy drugs – decitabine and panobinostat – to unlock tightly packed DNA molecules in glioblastoma cells. This unlocking triggered transposable elements to create the unusual proteins that could make the cancer cells visible to immune attack.
Challenges and Future Directions
While the results show promise, the researchers acknowledge important challenges ahead. The study revealed that normal cells also produced some targets when exposed to the drugs, though fewer than cancer cells. This potential side effect needs careful consideration before moving to clinical trials.
The research team is now investigating using CRISPR molecular editing technology to target specific parts of cancer cells’ genomes, aiming to produce neoantigens while sparing healthy cells.
“Immunotherapy has revolutionized the treatment of some specific cancers, such as melanoma,” said Kim, who treats patients at Siteman Cancer Center. “Progress in glioblastoma has been slow by comparison because of how resistant this tumor is to the latest therapeutic strategies. But with recent advancements in immunotherapies and epigenetic therapies that could be used in combination, I’m hopeful that we are on the right path for a similar transformative change in the treatment of glioblastoma.”
Glossary
• Glioblastoma: An aggressive type of brain cancer with typically poor survival rates
• Epigenome: The system that controls which genes are turned on in a cell and to what degree
• Transposable elements: Segments of DNA that can change position within a genome
• Neoantigens: Unique proteins produced by tumor cells that can be recognized by the immune system
• CRISPR: A precise molecular tool for editing genes
Reader Comprehension Quiz
1. What is the main challenge in treating glioblastoma with immunotherapy?
Answer: Glioblastoma cells have few or no natural targets for the immune system to attack.
2. Which two FDA-approved drugs were used in the study?
Answer: Decitabine and panobinostat
3. What is the role of transposable elements in this research?
Answer: They can produce unique proteins (neoantigens) that could serve as targets for immunotherapy.
4. What is the main concern that needs to be addressed before clinical trials?
Answer: Normal cells also produce some targets when exposed to the drugs, which could cause unwanted side effects.
Enjoy this story? Get our newsletter! https://scienceblog.substack.com/