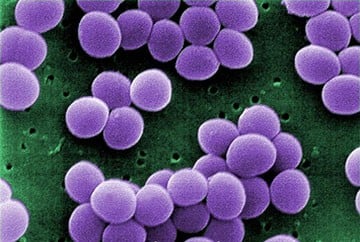
The pain of invasive skin infections caused by methicillin-resistant Staphylococcus aureus, and possibly other serious, painful infections, appear to be induced by the invading bacteria themselves, and not by the body’s immune response as previously thought, report scientists at Boston Children’s Hospital.
What’s more, their research demonstrates that once the pain neurons “sense” the bacteria, they suppress the immune system, potentially helping the bacteria become more virulent.
The study, conducted in a mouse model and published in Nature on August 21, could change the way doctors think about a variety of invasive, painful infections, such as meningitis, necrotizing fasciitis, urinary tract infections, dental caries and intestinal infections.
“If we could block pain in infected tissues and also block what pain neurons do to the immune system, it could help us treat bacterial infections better,” says Isaac Chiu, the study’s first author and a neuro-immunologist in the laboratory of Clifford Woolf, Harvard Medical School professor of neurobiology at Boston Children’s F.M. Kirby Neurobiology Program.
The study was launched after Chiu and coauthor Christian A. Von Hehn, were culturing sensory neurons and immune cells together in a dish to see how they interact during an infection. “Surprisingly, the neurons were responding immediately to the bacteria,” says Chiu.
That inspired them to move to a live model of skin infection, the first one to their knowledge ever used to study pain, working closely with Balthasar Heesters, a graduate student in the lab of Michael Carroll, in the Program in Cellular and Molecular Medicine at Boston Children’s.
The finding that pain neurons, once activated by bacteria, suppress the immune system was equally unexpected. “I was thinking they would do the opposite,” says Chiu.
Why would the activated pain neurons try to weaken the immune response to infection? Chiu hypothesizes that the neurons are trying protect tissues from further damage caused by an inflammatory immune response—a protective mechanism that bacteria might be exploiting to their advantage.
In the study, Chiu and colleagues examined pain, tissue swelling, immune cell numbers and the number of live bacteria in mice with staphylococcal skin infections. They found that pain levels tracked closely with the number of live bacteria and peaked well before tissue swelling peaked, in keeping with bacteria being the cause of the pain and not a local inflammatory response. The team also documented communication between bacteria, pain neurons and key cells from the immune system.
Bacteria “talk to neurons”
The research showed that S. aureus bacteria secrete two kinds of compounds that communicate with sensory neurons, inducing pain:
· N-formyl peptides: Pain neurons carry receptors to detect these peptides, known as FPR1 receptors, the team demonstrated. When mice are unable to make these receptors, they show a reduced pain response.
· Pore-forming toxins: These proteins, also secreted by other virulent bacteria, dock on the sensory nerve terminals and create large pores that let ions into the cells—triggering them to fire off pain messages. A pore-forming toxin known as alpha toxin is known to help S. aureus spread in the skin and lungs.
These findings suggest possible new approaches for blocking pain signaling by blocking the FPR1 receptor, blocking the receptor for alpha-toxin (ADAM10) on sensory neurons or possibly delivering a drug through the pores. These approaches also might prevent the neurons from suppressing the immune response, Chiu says, but this has yet to be proven.
Suppressing the immune system
Further experiments in mice demonstrated two ways in which the activated sensory neurons suppress the immune response at the local infection site, potentially allowing bacteria to proliferate:
· Innate immunity: Activated pain-sensing neurons reduce the influx of neutrophils and monocytes, key first responders to infection. In mice, when these neurons were eliminated through genetic techniques, numbers of these immune cells increased. The team further showed that the neurons talk to the immune cells via peptide molecules. One called CGRP, for example, prevented macrophages from producing TNF-alpha, a critical signal that rallies further immune defenses against bacteria.
· Draining lymph nodes: Normally, antigens from invading bacteria drain from the infection site to the lymph nodes, where T-cells and B-cells congregate and generate the body’s second-wave immune response. The team showed, however, that activated pain-sensing neurons reduce migration of T- and B-cells to the lymph nodes. In infected mice whose pain-sensing neurons were eliminated, the lymph nodes contained more of these cells.
The researchers plan to explore the pain-bacteria-immune system relationship further, and investigate treatments to block the pain caused by virulent bacterial infections, and perhaps to counter the immune suppression.
“We found that major parts of the immune system are not necessary for pain during infection, but that bacteria themselves are the source of much of the pain,” summarizes Chiu. “In treating pain during infection, we may need to think about how to block the pathogenic components themselves, and not just the immune/inflammatory pathways. We also found that sensory neurons modulate the immune system after they’re activated. This suggests, though we haven’t yet been able to prove it, that the ability of virulent bacteria strains to cause pain may give them an advantage, by allowing them to use the neurons to suppress immunity.”
The study was supported by the National Institutes of Health (PO1AI078897, 5RO1AI039246, R37NS039518, 5P01NS072040, 5F32NS076297) and Boston Children’s Hospital’s IDDRC facilities (NIH-P30-HD018655). Coauthors were Balthasar Heesters and Michael Carroll of the Program in Cellular and Molecular Medicine; Nader Ghasemlou, Christian Von Hehn, Fan Zhao, Johnathan Tran, Brian Wainger, Amanda Strominger, Sriya Muralidharan and Sun Wook Hwang of Boston Children’s Hospital; Alexander Horswill of the University of Iowa; and Juliane Bubeck Wardenburg of the University of Chicago.