In developing nations, rural areas, and even one’s own home, limited access to expensive equipment and trained medical professionals can impede the diagnosis and treatment of disease. Many qualitative tests that provide a simple “yes” or “no” answer (like an at-home pregnancy test) have been optimized for use in these resource-limited settings. But few quantitative tests—those able to measure the precise concentration of biomolecules, not just their presence or absence—can be done outside of a laboratory or clinical setting. By leveraging their discovery of the robustness of “digital,” or single-molecule quantitative assays, researchers at the California Institute of Technology (Caltech) have demonstrated a method for using a lab-on-a-chip device and a cell phone to determine a concentration of molecules, such as HIV RNA molecules, in a sample. This digital approach can consistently provide accurate quantitative information despite changes in timing, temperature, and lighting conditions, a capability not previously possible using traditional measurements.
In a study published on November 7 in the journal Analytical Chemistry, researchers in the laboratory of Rustem Ismagilov, Ethel Wilson Bowles and Robert Bowles Professor of Chemistry and Chemical Engineering, used HIV as the context for testing the robustness of digital assays. In order to assess the progression of HIV and recommend appropriate therapies, doctors must know the concentration of HIV RNA viruses in a patient’s bloodstream, called a viral load. The problem is that the viral load tests used in the United States, such as those that rely on amplification of RNA via polymerase chain reaction (PCR), require bulky and expensive equipment, trained personnel, and access to infrastructure such as electricity, all of which are often not available in resource-limited settings. Furthermore, because it is difficult to control the environment in these settings, viral load tests must be “robust,” or resilient to changes such as temperature and humidity fluctuations.
Many traditional approaches for measuring viral load involve converting a small quantity of RNA into DNA, which is then multiplied through DNA amplification—allowing researchers to see how much DNA is present in real time after each round of amplification, by monitoring the varying intensity of a fluorescent dye marking the DNA. These experiments—known as “kinetic” assays—result in a readout reflecting changes in intensity over time, called an amplification curve. To find the original concentration of the beginning bulk RNA sample, the amplification curve is then compared with standard curves representing known concentrations of RNA. Since assays, such as those for HIV, require many rounds of DNA amplification to collect a sufficiently bright fluorescent signal, small errors introduced by changes in environmental conditions can compound exponentially—meaning that these kinetic measurements are not robust enough to withstand changing conditions.
In this new study, the researchers hypothesized that they could use a digital amplification approach to create a robust quantitative technique. In digital amplification, a sample is split into enough small volumes such that each well contains either a single target molecule or no molecule at all. Ismagilov and his colleagues used a microfluidic device they previously invented, called SlipChip, to compartmentalize single molecules from a sample containing HIV RNA. SlipChip is made up of two credit card-sized plates stacked atop one another; the sample is first added to the interconnected channels of the SlipChip, and with a single “slip” of the top chip, the channels turn into individual wells.
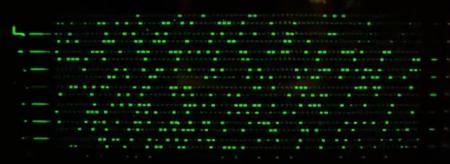
In lieu of PCR, the researchers used a different amplification chemistry on this chip called digital reverse transcription-loop-mediated amplification (dRT-LAMP), which produces a bright fluorescent signal in the presence of a target molecule during the amplification process. The dRT-LAMP technique eliminates the need for continuous tracking of the intensity of fluorescence; instead, just one end-point readout measurement is used. The resulting patchwork of “positive” or “negative” wells on the device, in combination with statistical analysis, enables single molecules to be counted.
“In each well, you are performing a qualitative experiment; the result is like a pregnancy test: either yes or no, positive or negative, for the presence of an HIV RNA molecule,” says David Selck, a graduate student in Ismagilov’s lab and a first author on the study. “But by doing a couple of thousand qualitative experiments, you end up getting a numerical, quantitative result: the concentration of HIV RNA molecules in the sample. By calculating the concentration from the number of wells that contain fluorescence—and therefore HIV—you’re leveraging the robustness of many qualitative ‘yes or no’ experiments to fulfill the need for a quantitative, numerical result,” he says.
When the researchers compared quantification results from dRT-LAMP to those obtained by the real-time, kinetic version of this chemistry, RT-LAMP, they found that the digital format provided accurate results despite changes in temperature and time, while the kinetic format could not. This finding adds to a body of research that the laboratory has been developing on the robustness of converting analog signals (i.e., a readout reflecting a changing concentration over time) into a series of positive or negative digital signals. Another recent paper, published in the Journal of the American Chemical Society, explored a variation on this analog-to-digital conversion.
Ismagilov’s group also tested a way to take an image of the fluorescence pattern in the wells of the SlipChip and, from that image, determine the viral load—without the use of expensive microscopes or trained staff. They turned to a nearly ubiquitous 21st-century technology: the smartphone.
The researchers placed the SlipChip in a makeshift darkroom (a shoebox with a hole in the top) and then photographed its wells using a smartphone outfitted with a special filter attachment—so that the smartphone flash would be able to “excite” the fluorescent DNA dye, and the smartphone camera could capture an image of the fluorescence. The resulting images were uploaded to Microsoft SkyDrive, a cloud-based server, where custom software—designed by the researchers—determined the viral load concentration and sent the results back in an email. These capabilities allow the digital approach to perform reliably with automated processing, regardless of how poor the imaging conditions may be. As an example of its simplicity, a 5-year-old child was able to use this cell phone imaging method to obtain quantitative results using strands of RNA extracted from a noninfectious virus (a video of this demonstration is available on the Ismagilov lab’s YouTube channel).
“We were surprised that this cell phone method worked, because both cell phone imaging and automated processing are error prone,” Ismagilov says. “Because digital assays involve simply distinguishing positives from negatives, we found that even these error-prone approaches can be used to count single molecules reliably.”
The fact that this method is robust not only to changes in time and temperature but also is amenable to cell phone imaging and automated processing makes it a promising technology for limited-resource settings. “We believe that our findings of the robustness of digital amplification could signal a major paradigm shift in how quantitative measurements are obtained at home, in the field, and in developing countries,” Ismagilov says.
The researchers stress that there is still room for improvement, however. “While in this study we were examining robustness and used purified RNA, the next generation of devices will isolate HIV RNA molecules directly from patients’ blood,” says Bing Sun, a graduate student in Ismagilov’s lab and a first author on the study. “We will also adapt the devices for other viruses, such as hepatitis C. By combining these improvements with the cell phone imaging method, we plan to create something that could actually be used in the real world,” Sun adds.
 The paper is titled “Increased Robustness of Single-Molecule Counting with Microfluidics, Digital Isothermal Amplification, and a Mobile Phone versus Real-Time Kinetic Measurements.” In addition to Selck, Sun, and Ismagilov, the paper is coauthored by Mikhail A. Karymov, an associate scientist at Caltech. The work was funded by the Defense Advanced Research Projects Agency award number HR0011-11-2-0006, and by the National Institutes of Health award numbers R01EB012946 and 5DP1OD003584. Microfluid technologies developed by Ismagilov’s group have been licensed to Emerald BioStructures, Randance Technologies, and SlipChip LLC.
The paper is titled “Increased Robustness of Single-Molecule Counting with Microfluidics, Digital Isothermal Amplification, and a Mobile Phone versus Real-Time Kinetic Measurements.” In addition to Selck, Sun, and Ismagilov, the paper is coauthored by Mikhail A. Karymov, an associate scientist at Caltech. The work was funded by the Defense Advanced Research Projects Agency award number HR0011-11-2-0006, and by the National Institutes of Health award numbers R01EB012946 and 5DP1OD003584. Microfluid technologies developed by Ismagilov’s group have been licensed to Emerald BioStructures, Randance Technologies, and SlipChip LLC.