Men with hormone-sensitive metastatic prostate cancer who received the chemotherapy drug docetaxel given at the start of standard hormone therapy lived longer than patients who received hormone therapy alone, according to early results from a National Institutes of Health-supported randomized controlled clinical trial.
The independent Data and Safety Monitoring Committee overseeing the trial recommended to the National Cancer Institute (NCI), part of NIH, that the study results be made public because a recent planned interim analysis showed the prolongation in overall survival. Full details from this early analysis will be presented at a scientific meeting in 2014 and in a peer-reviewed publication.
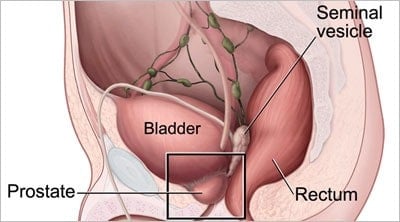
The study enrolled 790 men with metastatic prostate cancer between July 2006 and November 2012 in a trial known as E3805. All patients started treatment by receiving a form of hormone therapy known as ADT (androgen deprivation therapy). Androgens regulate male sex characteristics and can stimulate prostate cancer cells.
Men received either ADT alone or ADT with the chemotherapy drug docetaxel every three weeks over a period of 18 weeks. In addition to examining whether the study participants lived longer with the addition of chemotherapy, investigators looked at whether the extent of a patient’s metastatic disease was high or low at the start of treatment. Approximately two thirds of patients had a high extent of disease which, according to the study, meant the disease had spread to major organs such as the liver, had a spread resulting in four or more bone lesions, or both.
A significant improvement in the overall survival was noted favoring the participants who had received docetaxel chemotherapy in addition to the ADT compared to the ADT alone (three-year survival rates of 69.0 percent vs. 52.5 percent respectively). Further analysis showed that patients with a high extent of metastatic disease accounted for most of the benefit in the overall survival from docetaxel plus ADT (three-year survival rates of 63.4 percent vs. 43.9 percent for ADT alone). Median follow-up to date is two years.
Since docetaxel has been shown in previous clinical trials to be beneficial in ADT-resistant disease and is approved by the U.S. Food and Drug Administration for treatment of late-stage prostate cancer, it is available for use now. However, because it is a chemotherapy drug associated with some toxicities, its use in combination with ADT at this time should be restricted to patients with high-extent metastatic prostate cancer who are candidates for treatment with docetaxel, according to the trial investigators. This is the group of patients who experienced the most benefit in the current analysis. Further follow-up will be performed on patients with less extensive metastatic disease who participated in E3805 in order to define the effect of this treatment combination on these patients.
“The results of this study are practice-changing,” said lead investigator Christopher Sweeney, Dana Farber Cancer Institute, Boston. “We have strong scientific evidence that patients with the most advanced metastatic prostate cancer benefit from the early addition of docetaxel to ADT and not waiting until the cancer has progressed on hormonal therapy. The findings of this study are important both for improving the clinical care we deliver now and in designing new clinical trials as we strive to further improve the lives of men with metastatic prostate cancer.”
E3805 was sponsored by NCI and was designed and conducted by the ECOG-ACRIN Cancer Research Group in collaboration with SWOG, Alliance for Clinical Trials in Oncology, and NRG Oncology. Sanofi, Paris, the drug manufacturer, provided the docetaxel and supported this study under a Clinical Trials Agreement with ECOG-ACRIN.
“This trial would not have been done in the United States without a large national network of investigators brought together through the NCI-supported Cooperative Group program that was capable of rapidly enrolling many patients,” said Jeff Abrams, M.D., clinical director of NCI’s Division of Cancer Treatment and Diagnosis. “Additionally, these findings are an example of how combining two approved and available treatments can produce a significant improvement in clinical outcome.
 It is estimated that over 238,000 men will be diagnosed with prostate cancer in the United States in 2013 and over 29,000 men will die of the disease.
It is estimated that over 238,000 men will be diagnosed with prostate cancer in the United States in 2013 and over 29,000 men will die of the disease.
NCI leads the National Cancer Program and the NIH effort to dramatically reduce the prevalence of cancer and improve the lives of cancer patients and their families, through research into prevention and cancer biology, the development of new interventions, and the training and mentoring of new researchers. For more information about cancer, please visit the NCI website at http://www.cancer.gov or call NCI’s Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.