A new paper is the first to report that specialized fat (lipid) molecules, called sphingolipids, play a key role in the survival of aggressive lymphomas caused by viruses.
The paper, whose senior author is Christopher Parsons, MD, Director of the HIV Malignancies Program at LSU Health Sciences Center New Orleans, also reveals a new therapy for preventing production of sphingolipids by lymphoma cells, thereby killing these cells, which are often resistant to standard therapies. The study is published in the January 2014 issue of Molecular Cancer Therapeutics, a journal of the American Association for Cancer Research.
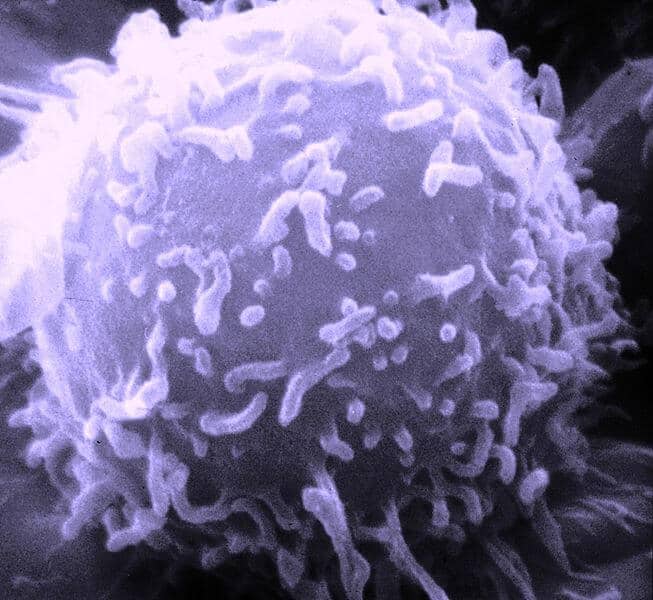
The research team focuses on primary effusion lymphoma (PEL), an aggressive and deadly variant of diffuse large B-cell lymphoma that frequently occurs in people infected with HIV. Though scientists have known that the Kaposi’s sarcoma-associated herpesvirus (KSHV) causes PEL, development of effective therapies has proven difficult. PEL tumors arise within body cavities and progress rapidly with an average survival of around 6 months. Combination chemotherapy represents the current standard of care for PEL, but side effects (including bone marrow suppression) and drug resistance (generated through virus-associated mechanisms) continue to limit the effectiveness of standard therapy.
After documenting the role of an enzyme called sphingosine kinase (SK), in the generation of biologically active sphingolipids in PEL tumors that keep the tumor cells alive, the researchers tested a novel clinical-grade small molecule that selectively targets SK. The molecule, called ABC294640, was developed by Apogee Biotechnology Corporation. Previous studies found antitumor effects for ABC294640 with kidney, prostate, and breast cancer cell lines. In the current study, ABC294640 not only inhibited SK function and induced PEL cell death, it worked selectively for virus-infected cells while sparing uninfected cells.
“It is still early in our understanding of how these special lipids contribute to viral cancers, but this is a major potential advance. There are no therapies available to fight viral tumors by selectively blocking these pathways, all while not harming normal, uninfected cells,” notes Dr. Parsons, who is also a member of the LSUHSC Stanley S. Scott Cancer Center.
Dr. Parsons’ research group partnered with Apogee several years ago to develop and test new small molecules targeting lipid synthesis pathways, especially those in viral lymphomas, which have high rates of relapse or failure with standard therapies and higher mortality than non-viral lymphomas.
“Our research thus far indicates that this molecule is safe, with the potential to stand alone as a single, orally administered drug with no need to combine it with other toxic drugs now routinely used but which fail to work for many patients,” concludes Dr. Parsons.