Findings by Cincinnati Cancer Center researchers show that levels of bisphenol A (BPA) in men’s urine could be a marker of prostate cancer and that low levels of BPA exposure can cause cellular changes in both non-malignant and malignant prostate cells.
This research, published in the March 3 edition of PLOS ONE, provides the first evidence that urinary BPA levels may help predict prostate cancer and that disruption of a cell duplication cycle through exposure to low-dose BPA may cause cancer development in the prostate.
BPA, an environmental pollutant with estrogen activity, is used to make hard, clear plastic and is common in many food product containers. It has been linked to neurological defects, diabetes and a number of cancers, including breast and prostate.
Principle investigator Shuk-mei Ho, PhD, director of the Cincinnati Cancer Center, Jacob G. Schmidlapp Chair of Environmental Health and professor at the University of Cincinnati College of Medicine, says that human exposure to BPA is a common occurrence and that animal studies have shown that BPA contributes to development of prostate cancer but that human data are scarce.
“Prostate cancer is the second most common cancer among men in North America, and one in six men will develop it over their lifetime,” she says. “However, the cancer is rarely diagnosed in men under the age of 40 with almost two-thirds of cases reported in men at age 65.
“Major contributing factors other than age are race and family history, whereas little is known about the impact of endocrine disruptors on prostate cancer.”
Ho says that in the United States, exposure to BPA is widespread—exceeding 90 percent in the general population—and that absorption through the skin, inhalation and ingestion from contaminated food and water are the major kinds of exposure.
“As an endocrine disruptor that mimics estrogen and thyroid hormones, BPA also acts as a metabolic and immune disruptor,” says Ho. “The adverse health effects of BPA are extensive, and studies in animals have proven this”.
“However, human studies linking BPA exposure to heightened cancer risk are limited,” she continues. “Our study examined the association between urinary BPA levels and prostate cancer and assessed the effects of BPA on the initiation of centrosome abnormalities as an underlying mechanism promoting prostate cancer formation.”
A centrosome is an organelle required for proper cell division, and centrosome abnormalities are frequently observed in cancers.
In the study, researchers assessed the PSA of 60 urology patients using urine samples. Higher levels of BPA were found in prostate cancer patients than in non-prostate cancer patients (5.74 μg/g creatine versus 1.43 μg/g creatine), and the difference was even more significant in patients less than 65 years of age.
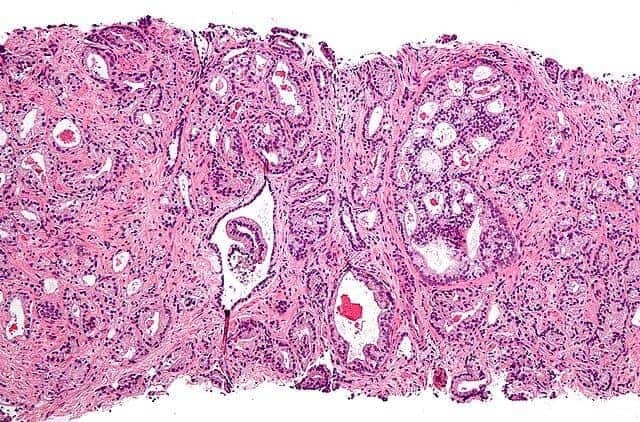
Additionally, researchers examined prostate cells—normal and cancerous—using immunofluorescence, allowing them to visualize the distribution of the target molecule and look specifically at centrosomal abnormalities and growth patterns.
“Exposure to low doses of BPA increased the percentage of cells with centrosome amplification two- to eight-fold,” Ho says. “BPA is not a recognized carcinogen, and questions surrounding the mechanism behind the positive correlation of BPA exposure with prostate cancer have arisen”.
“Several studies have shown that centrosome amplification is a major contributing factor to chromosomal mutation in human tumors. We examined the centrosome profile of prostate cancer cells treated with BPA and found that treatment with BPA increased the number of cells with abnormal centrosomes”.
“All of these findings reveal a previously unknown relationship between BPA exposure and prostate cancer and suggest a mechanism underlying the role of BPA in cellular transformation and disease progression. With this insight, we hope to further investigate ways we can decrease exposures to potentially cancerous-causing chemicals in every day products and substances and reduce the onset of prostate cancer in men.”