Most people appreciate that not getting enough sleep impairs cognitive performance. For the chronically sleep-deprived such as shift workers, students, or truckers, a common strategy is simply to catch up on missed slumber on the weekends. According to common wisdom, catch up sleep repays one’s “sleep debt,” with no lasting effects. But a new Penn Medicine study shows disturbing evidence that chronic sleep loss may be more serious than previously thought and may even lead to irreversible physical damage to and loss of brain cells. The research is published today in The Journal of Neuroscience.
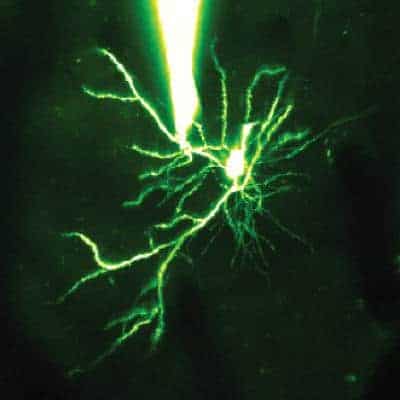
Using a mouse model of chronic sleep loss, Sigrid Veasey, MD , associate professor of Medicine and a member of the Center for Sleep and Circadian Neurobiology at the Perelman School of Medicine and collaborators from Peking University, have determined that extended wakefulness is linked to injury to, and loss of, neurons that are essential for alertness and optimal cognition, the locus coeruleus (LC) neurons.
“In general, we’ve always assumed full recovery of cognition following short- and long-term sleep loss,” Veasey says. “But some of the research in humans has shown that attention span and several other aspects of cognition may not normalize even with three days of recovery sleep, raising the question of lasting injury in the brain. We wanted to figure out exactly whether chronic sleep loss injures neurons, whether the injury is reversible, and which neurons are involved.”
Mice were examined following periods of normal rest, short wakefulness, or extended wakefulness, modeling a shift worker’s typical sleep pattern. The Veasey lab found that in response to short-term sleep loss, LC neurons upregulate the sirtuin type 3 (SirT3) protein, which is important for mitochondrial energy production and redox responses, and protect the neurons from metabolic injury. SirT3 is essential across short-term sleep loss to maintain metabolic homeostasis, but in extended wakefulness, the SirT3 response is missing. After several days of shift worker sleep patterns, LC neurons in the mice began to display reduced SirT3, increased cell death, and the mice lost 25 percent of these neurons.
“This is the first report that sleep loss can actually result in a loss of neurons,” Veasey notes. Particularly intriguing is, that the findings suggest that mitochondria in LC neurons respond to sleep loss and can adapt to short-term sleep loss but not to extended wake. This raises the possibility that somehow increasing SirT3 levels in the mitochondria may help rescue neurons or protect them across chronic or extended sleep loss. The study also demonstrates the importance of sleep for restoring metabolic homeostasis in mitochondria in the LC neurons and possibly other important brain areas, to ensure their optimal functioning during waking hours.
Veasey stresses that more work needs to be done to establish whether a similar phenomenon occurs in humans and to determine what durations of wakefulness place individuals at risk of neural injury. “In light of the role for SirT3 in the adaptive response to sleep loss, the extent of neuronal injury may vary across individuals. Specifically, aging, diabetes, high-fat diet and sedentary lifestyle may all reduce SirT3. If cells in individuals, including neurons, have reduced SirT3 prior to sleep loss, these individuals may be set up for greater risk of injury to their nerve cells.”