Blood vessels have been thought to be important to cancer because of the nutritious oxygen they provide to growing tumors. But now, researchers at Weill Cornell Medical College have discovered that the cells that line the blood vessels of tumors play a much more decisive role: By producing proteins that nurture cancer, the vessels have the ability to turn a slow-growing malignancy into an aggressive disease that can spread and resist treatment.
Their finding, in the March 17 issue of Cancer Cell , challenges what was believed to be a fundamental dogma in cancer. It suggests that it is not simply the number of genetic mutations that occur in cancer cells that determines the aggressiveness of the disease. Rather, lethality occurs when the cancer hijacks the reparative function of blood vessels, a critical step that ensures tumor cells’ ability to spread and resist treatment.
The researchers also found the crucial nurturing molecules that cancer co-opts from tumor blood vessels to promote invasiveness and resistance to chemotherapy. They show in animal experiments that shutting down these previously unrecognized biological signals originating from tumor vessels makes cancer less aggressive and improves survival.
“The endothelial cells that line the vessels orchestrate a wide variety of biological processes — good and bad,” says the study’s senior investigator, Dr. Shahin Rafii, co-director of Weill Cornell’s Ansary Stem Cell Institute and Tri-Institutional Stem Cell Initiative, and a professor of Genetic Medicine. Dr. Rafii also is the founder of Angiocrine Bioscience, a startup anchored at Weill Cornell that is investigating how endothelial cells might be used to heal damaged tissues and regenerate organs – as well as target tumors. “The understanding and control of blood vessel function and how this changes the malignant behaviors of cancer cells is a transformative concept and will pave the way for designing innovative treatments that disrupt signals from the local environment housing the tumor cells- a strategy that has been unappreciated.”
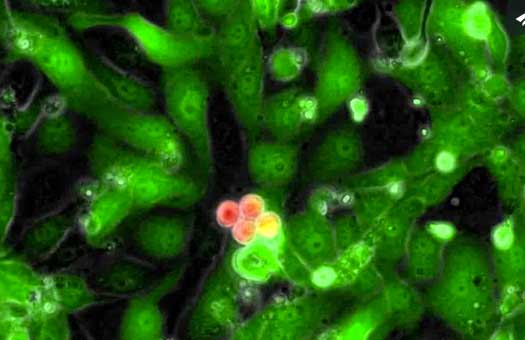
The scientists studied human B cell lymphoma cells in both laboratory experiments and in mice. They found that although the lymphoma cells harbor the same mutations, it is their interaction with and support from the tumor blood vessel cells that surround the cancer that dictates the fate and features of the disease.
Specifically, when slow-growing tumor cells contact endothelial cells that express a protein known as Jagged 1 (Jag 1), “they become much more aggressive and resistant to chemotherapy,” says the study’s lead investigator, Dr. Zhongwei Cao, a research scientist in the Department of Genetic Medicine at Weill Cornell. “When Jagged 1 is not available from surrounding blood vessels, the lethal features of tumor cells are absent.”
They further found that when Jag1 binds to and activates a receptor, Notch2, on tumor cells, the cancer becomes more tolerant of chemotherapy. “These tumor cells are sheltered from chemotherapy,” Dr. Cao says.
The researchers, joined by colleagues at Stanford and Yale, also identified how interactions between the tumor cells and the blood vessels confer these tumor cells with their aggressive and lethal features. “We think signals from these abnormally stimulated tumor endothelial cells modulate the malignant features of lymphoma cells. This is a reversible process dictated by the location of the tumor cells rather than their genetics,” says Dr. Joseph Scandura, an assistant professor of medicine at Weill Cornell. “This is a critical finding because it suggests that targeting the endothelial cells with agents that disrupt their specific pro-tumorigenic signals can transform aggressive cancers into slow-growing cancers that are more sensitive tochemotherapy.”
The researchers found, for example, that blocking the Notch2 receptor in lymphoma cells or Jag1 on blood vessels made the lymphoma cells significantly more vulnerable to chemotherapy. Even though the experiment was conducted using lymphoma cells, “we expect this finding to be applicable to other cancers, as well,” says Dr. Bi-Sen Ding, co- senior investigator of the study and an assistant professor of genetic medicine at Weill Cornell.
“This new approach to treatment would interfere with the nurturing proteins produced by tumor blood vessels. It is different from traditional anti-angiogenic therapy that aims to eradicate all blood vessels in the tumor and prevent them from bringing oxygen and nutrients to the cancer,” says Dr. Ding, noting that conventional anti-angiogenic therapy can increase the aggressiveness of certain tumor cells by paradoxically enhancing the expansion of tumor blood vessels. “Simply blocking specific proteins produced by tumor blood vessels, such as Jag1, without altering oxygen and nutrient delivery will avoid this problem.
“Our approach could readily be translated to the clinical setting since we can target tumor blood vessels by delivering biological cruise missiles loaded with inhibitory agents for specific cancer-promoting proteins to block tumor growth and increase sensitivity to chemotherapy,” Dr. Ding adds.
Finally, these studies suggest that screening for anti-cancer drugs may be more effective if tumor cells are assayed in the context of signals derived from the subverted blood vessels.