Limiting a certain protein in the brain reverses Alzheimer’s symptoms in mice, report neuroscientists at MIT’s Picower Intitute for Learning and Memory.
Researchers found that the overproduction of the protein known as p25 may be the culprit behind the sticky protein-fragment clusters that build up in the brains of Alzheimer’s patients. The work, which was published in the April 10 issue of Cell, could provide a new drug target for the treatment of the disease that affects more than five million Americans, says Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory and senior author of the paper.
Abnormal clusters of protein fragments, known as beta amyloid plaques, are believed to cause the cognitive impairments, cell death, and tissue loss associated with Alzheimer’s. The p25 protein had been tied to the creation and buildup of beta amyloids, but until now, p25’s role in Alzheimer’s pathology was not well understood.
“This protein appears to help maintain normal brain activity, but also is part of a feedback loop with beta amyloids. It generates the plaques which, in turn, boost levels of p25,” Tsai says.
Lead author of the paper is Jinsoo Seo, a postdoc associate at the Picower Institute.
The benefits of p25 generation
Elevated p25 levels in the brain have been documented upon exposure to neurotoxic stimuli such as oxidative stress and beta amyloids.
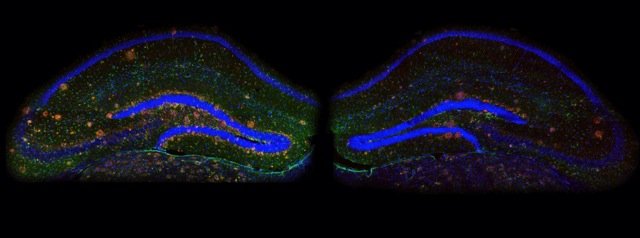
“In this study, for the first time we show that a variety of physiological neuronal activities generate p25 in the hippocampus, where memories are encoded in the brain,” Tsai says.
To delineate the precise roles of p25, Tsai’s lab generated a transgenic mouse model, which enabled researchers to prevent the production of p25 without altering other proteins with essential roles in brain development.
The researchers found that p25 is required for synaptic plasticity, the ability of brain connections to change over time; especially for the process called long-term depression (LTD) that selectively weakens sets of synapses and is associated with memory extinction.
Tsai’s team observed that the mice unable to generate p25 could learn new tasks and form memories normally; however, when the researchers began to address memory extinction, they soon noticed that the mice have difficulties with replacing older memories with newer ones.
Too much of a good thing
“This finding not only boosts our understanding of p25 in synaptic functions, but also explains the underlying mechanism of the inordinate synaptic depression observed in the Alzheimer’s brain,” Seo says.
“This finding led us to question whether the blockade of p25 generation could mitigate pathological phenotypes in the Alzheimer’s brain,” Tsai says.
In the mouse model of Alzheimer’s disease, inhibiting p25 production improved cognitive function, greatly reduced plaque formation and neuroinflammation, hallmark features of Alzheimer’s disease.
These results hold out the hope that a drug that regulates p25 could benefit Alzheimer’s disease patients by improving cognitive function and perhaps delaying the development of brain pathology, Tsai says. This work was supported in part by the National Institutes of Health and the Howard Hughes Medical Institute.


Is this sort of treatment also viable for other neurodegenerative diseases such as Parkinson’s disease? Seen as though there is a build up of protein is it possible for p25 to regulate autophagy pathways? With the medical field as it stands research such as this one is going to become more common which will greatly improve the pharmaceutical field as we know it, especially in those previously known ‘incurable’ diseases.
The discovery made by neuroscientists at MIT’s Picower Intitute for Learning and Memory, will definitely become the leading frontier in developing a pharmaceutical drug against Alzheimer’s. With the inhibition of the p25 protein production in Alzheimer affected patients, the formation of beta amyloid plaques will greatly be reduced and the resultant cognitive functioning of the individual will greatly increase; possibly the first viable treatment for Alzheimer patients in light of their dilapidated cognitive abilities. However this inhibition is not without consequence as synaptic weaknesses and the rigidity of synaptic pathways will become evident with the inhibition of this protein. Memory loss and a “weak memory” will still not be cured but this groundbreaking discovery is however a great step forward in better understanding the mechanisms of Alzheimer’s and could potentially be the first viable step in producing medicine that would not only give health practitioners better means for treating Alzheimer’s, but also patients all across the world a new sense of freedom and rehabilitation.