Efforts to reduce and stop the spread of infections caused by a highly resistant organism, carbapenem-resistant Acinetobacter baumannii, at a large Florida hospital proved ineffective until they added another weapon – weekly emails from the medical director of Infection Control to hospital leadership, according to a study published in the May issue of the American Journal of Infection Control, the official publication of the Association for Professionals in Infection Control and Epidemiology (APIC).
When the hospital added the step of sending comprehensive weekly reports to physician, hospital nursing, medical, and administrative leadership, the rate of A. baumannii transmission decreased by 63 percent, according to the research team from the University of Miami Miller School of Medicine. Prior to this, endemic rates of A. baumannii had been present at the institution for nearly two decades.
“These regular highly visible communications allowed us to create a sense of accountability for new cases that unified both the leadership and providers toward the common goal of decreasing new acquisitions of carbapenem-resistant A. baumannii,” state the study authors.
The study analyzed a 42-month period of hospital data (January 1, 2010 to June 30, 2013) representing 1.1 million patient days. During Phase 1 (2010-2011), the bundle of interventions had been implemented but rates had not changed. During Phase 2 (2011-2012), the medical director of Infection Control sent weekly emails to hospital leadership describing and interpreting the surveillance results from the previous week, including the number and location of newly discovered isolates; results of environmental cultures obtained from bed rails, bedside tables, intravenous pumps, and nursing stations; and a map indicating the location of carbapenem-resistantA. baumannii positive patients and objects. Two intensive care units (ICUs) with the highest rates received daily emails. During Phase 3 (2012-2013), the bundle of interventions continued but the weekly emails ceased because there were only scattered weekly acquisitions. Overall acquisition of new cases of carbapenem-resistant A. baumannii decreased from 5.13 per 10,000 patient days in Period 1, to 1.93 in Period 3.
“These weekly emails not only packaged information on the number and locations of new acquisitions of A. baumannii, but also described and explained the results of environmental initiatives, hand culture results, and identification of shared objects among patients,” add the authors. “Additionally, these communications advised the hospital and each ICU’s leaders about the infection control data and provided action plans based on the findings.”
The bundle of infection prevention measures included 1) patient screening tests upon admission to the ICU and weekly thereafter; 2) isolation and separation of patients testing positive for A. baumannii; 3) weekly sampling of surfaces in the hospital environment to assess thoroughness of cleaning; 4) hand hygiene interventions, including random cultures of healthcare workers’ hands, the results of which were included in the weekly reports; 5) observing shared objects that moved from patient-to-patient; and 6) monthly multidisciplinary meetings to discuss all issues related to implementing the bundle.
The authors conclude, “This is the first study to examine the effect of mass electronic dissemination of results from a bundle of interventions. Weekly electronic communications were associated with a striking decrease in the rate of new acquisitions of A. baumannii at our institution probably because of a combination of education, communication, feedback, and peer pressure.”
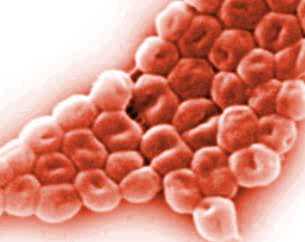
Acinetobacter baumannii is a type of gram-negative bacteria that is resistant to most antibiotics and has become one of the most worrisome and frequent organisms causing healthcare-associated infections in U.S. healthcare facilities.
Infections from A. baumannii occur mainly in intensive care units and affect primarily very ill, wounded, or immunocompromised patients. The germ can remain on wet or dry surfaces for longer than most other organisms, making it harder to eradicate. Multidrug-resistant Acinetobacter is classified as a serious threat by the Centers for Disease Control and Prevention.


I think this system should be implemented in South African hospitals, especially since the World Health Organisation recently released a statement saying that superbugs are increasing and more people are getting infected with superbugs. This system is inexpensive and will help decrease superbug infections. This is a great solution since medication to treat superbug infections will take 10 years to develop.
I think it is essential that the scientific community tries to find a way to reduce and stop the spread of infectious superbugs.
Since disease causing bacteria, that is resistant to antibiotics, are widespread through the world’s hospitals, it would be beneficial to both the patients and the hospital’s staff if other hospitals across the world also followed this large Florida hospital’s plan to stop the spread of superbugs. The threat that superbugs poses is so serious that it may endanger all that modern medicine have achieved. Patients in ICU units are already very vulnerable, since they are so ill. What use is it to be able to do a heart transplant for a patient if he have a serious chance of being infected with a superbug?
For this hospital to have lowered the amount of new cases of carbapenem-resistant A. Baumannii from 5.13 per 10,000 patient days to 1.93 per 10,000 patient days is an incredible achievement.