By targeting RNA molecules that tangle and clump in the nervous systems of patients with the most common genetic form of amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease) and frontotemporal dementia (FTD), researchers have shown they can effectively limit those damaging elements in cells taken from patients. The results reported in the Cell Press journal Neuron on August 14th show that RNA is a viable drug target for the two overlapping and incurable neurodegenerative diseases. The abnormal proteins derived from that aberrant RNA might also serve as biomarkers in clinical trials to test the new ALS and FTD drug candidate and otherwise monitor the diseases, the new study finds.
ALS is caused by a progressive loss of motor neurons, leading to severe impairment of mobility, speech, swallowing, and respiratory function that is usually fatal within two to five years, the researchers explained. In FTD, brain regions that support higher cognitive function are affected instead to produce disabling changes in behavior, personality, and language. At present, no effective treatment is available for either condition. However, experts believe that a better understanding of the underlying disease processes will expedite the development of effective therapies, say Leonard Petrucelli of the Mayo Clinic and Matthew Disney of The Scripps Research Institute.
Indeed, Petrucelli, Disney, and their colleagues say that they were pleasantly surprised at how quickly they were able to identify a small molecule capable of interrupting the disease process in cells carrying the C9ORF72 gene. The disease variant is characterized by an expansion of repetitive DNA, which leads to the production of lengthy RNA tangles and the translation of abnormal proteins, both of which can apparently “set in motion distinct toxic chains of events that ultimately lead to neuronal death.”
When the neurodegeneration targets motor neurons, the result is ALS. When it happens in brain regions that support higher cognitive function, then FTD develops. In some cases, affected people show signs of both conditions, which made it clear to Petrucelli and Disney that the aberrant RNA molecules were attractive targets for fighting the diseases.
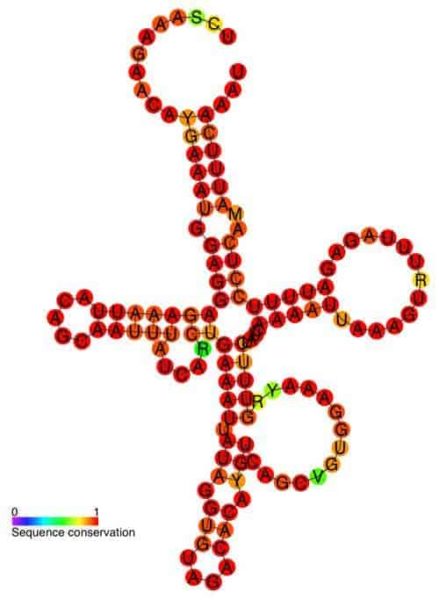
In search of promising small molecules for the job, the research team first examined the shape of the culprit RNA. The goal then was to identify compounds capable of binding to it, and they got lucky.
“We found that the RNA repeat that causes c9FTD/ALS has some structural similarities to the RNA that causes fragile X-associated tremor ataxia syndrome, to which we already identified a small molecule that could affect dysfunction,” Disney said.
By testing that compound and others that were chemically similar, they rather quickly identified two that selectively target c9FTD/ALS repeat RNA in cells. One of the two compounds cut the accumulation of RNA tangles in cell lines derived from ALS patients in half, they report, with no apparent toxicity. Petrucelli and Disney are now working on ways to improve it even further.
Importantly, the researchers also found that they could detect aberrant proteins in the spinal fluid of ALS patients with the C9ORF72 mutation, which might be useful when it comes to testing their compound or others in clinical trials.
“A decrease in the levels of c9RAN proteins in patient blood or cerebrospinal fluid in response to treatment would demonstrate the drug is working,” Petrucelli said. “While additional studies must be done, this finding suggests that c9RAN proteins may provide a direct means to measure a patient’s response to experimental drugs that target abnormal repeat RNA.”