A UB study has shown that high doses of steroids exert pro-inflammatory effects despite their use over the past six decades as anti-inflammatory drugs.
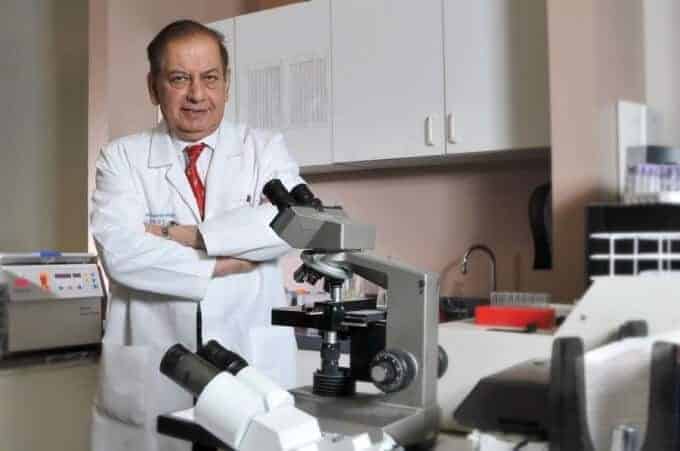
The study, led by Paresh Dandona, SUNY Distinguished Professor in the Department of Medicine and chief of endocrinology, diabetes and metabolism in the School of Medicine and Biomedical Sciences, is the first of its kind in humans, in vivo.
Dandona and fellow researchers found that high doses of corticosteroids — or steroids — have a primary anti-inflammatory effect. Yet, they also have certain pro-inflammatory effects that may limit their overall benefits.
“Our data show for the first time that corticosteroids lead to marked and persistent suppression of chemokines and several other inflammatory cytokines and mediators in humans, in vivo,” he explains.
Chemokines and cytokines are regulators of inflammatory responses and their suppression is a part of the anti-inflammatory action of steroids.
Therefore, the action of steroids on chemokines is immensely important, says Dandona.
At higher doses, steroids induce proteins and mediators such as toll-like receptors, which mediate responses to infectious agents and endotoxin, but also may lead to potentially harmful excessive inflammatory responses, he explains.
In addition, they induce the protein HMG-B1, an alarmin that, when increased in mice, is related to mortality after an injection of endotoxin. Steroids also cause an increase in plasma levels of glucose and free fatty acids, which are inflammatory and interfere with insulin action, inducing insulin resistance and promoting diabetes.
“There is a need for novel anti-inflammatory agents that are potent but do not exert harmful side effects,” he emphasizes.
While steroids are effective in many inflammatory conditions, they are ineffective — even when given in extremely high doses — in the treatment of septicemia, a state of severe inflammation often caused by overwhelming infection, Dandona notes.
On the other hand, he says several inflammatory conditions, like asthma and rheumatoid arthritis, respond to steroids, but when given in high doses, these drugs cause damaging side effects like obesity, high blood pressure and diabetes.
Most research in this field has been carried out on cell lines, in vitro or in experimental animals.
In Dandona’s study, however, 10 participants were injected with either saline or the steroid hydrocortisone during two separate visits. The researchers then obtained blood samples at 0, 1, 4, 6 and 24 hours after the injections.
Although steroids are the most common anti-inflammatory agents, scientists until now haven’t had much data about their actions in vivo, in humans, says Dandona.
“This is remarkable in the context of their potency, the frequency of their use, the duration that they have been in use — more than 50 years — and their known adverse effects,” he says.
In 2013, Dandona and fellow researchers discovered that insulin injections exert a strong anti-inflammatory effect at the cellular and molecular level.
“Since our previous work has shown that insulin suppresses the pro-inflammatory factors induced by corticosteroids, the observations from this study lay the foundations for an anti-inflammatory cocktail of steroids and insulin,” he says.
Such a combination would potentially have double the anti-inflammatory activity without the harmful side effects of steroids, he explains.
This combination could be used for any severe condition, such as acute asthma, and for inflammatory conditions requiring hospitalization.
The researchers note that because they observed the paradoxical pro- and anti-inflammatory effects in healthy subjects, further studies in actual clinical situations — including the life-threatening infection septicemia — are required.
The paper, “A Mixed Anti-Inflammatory and Pro-Inflammatory Response Associated With a High Dose of Corticosteroids,” has been published in Current Molecular Medicine.
Dandona’s co-authors in the Department of Medicine are Husam A. Ghanim, research assistant professor and senior research associate; Ajay Chaudhuri, clinical associate professor; Antoine Makdissi, clinical associate professor; Kelly Green, research assistant; and Sanaa I. Abuaysheh, research associate. Sandeep Dhindsa, a former faculty member, and Ching L. Sia, research associate, also are co-authors.
– See more at: http://www.buffalo.edu/ubreporter/research/news.host.html/content/shared/university/news/ub-reporter-articles/stories/2014/September/dandona_steroids.detail.html#sthash.A6oKMHgk.dpuf