The Centers for Disease Control and Prevention has said that at least 2 million Americans are sickened by antibiotic resistant infections each year and survive. (Twenty-three thousand die.) These experiences leave deep impressions not just on the patients but on their family and friends.
Michael Kinch, PhD, associate vice chancellor and director of the Center for Research Innovation in Business, is among that number. A few years ago his 12-year-old son suddenly became ill, so ill Kinch had to carry him into a nearby clinic in his arms. Because his son had a fever, the doctors at the clinic put him on first one and then a second antibiotic while they worked on a diagnosis.
They soon learned his son’s appendix had burst and he was septic. “Things moved so fast he was septic before he was symptomatic [for appendicitis],” Kinch said. His son was moved to an academic medical center where he had surgery and was put on four newer antibiotics.
When the lab tests for antibiotic susceptibility finally came in, they showed the pathogenic bacteria were susceptible to only two of the six antibiotics Kinch’s son had been given. Stunningly, the two that worked were the older drugs he had been given at the clinic. “I can only assume that if we had gone straight to the academic medical center, he might not have survived,” Kinch said.
“It’s not that my son had had extensive exposure to antibiotics,” Kinch explained carefully. “We’re all just colonized by resistant bacteria now.”
“Three weeks later I was asked to join a nonprofit organization working on new models for drug development, called the Institute for Life Sciences Collaboration,” Kinch said. “The institute was picking the therapeutic areas that would be their focus. “They were considering various exotic diseases, and I said, ‘Antibiotics.’”
Antibiotics are crashing
In his last position, as managing director of the Center for Molecular Discovery at Yale University, Kinch had assembled a huge database of information about drug discovery and development in the pharmaceutical industry. (See “‘The process by which drugs are discovered and developed will be fundamentally different in the future.’”)
He has been able to excavate story after story from this storehouse of data. The crash of antibiotics is one of the best known and scariest, since losing antibiotics would force changes in almost every area of medical practice. (See “In the media” for more information.)
In an article in Drug Discovery Today, Kinch summarized the financial constraints that have led to the current crisis in antibiotic supply. (See “An Analysis of FDA-approved drugs for infectious disease: antibacterial agents.”) The number of antibiotics available for clinical use, Kinch said, has declined to 96 from a peak of 113 in 2000.
The rate of withdrawals is double the rate of new introductions, Kinch said. Antibiotics are being withdrawn because they don’t work anymore, because they’re too toxic or because they’ve been replaced by new versions of the same drug. Introductions are declining because pharmaceutical companies are leaving the business of antibiotic discovery and development.
Pfizer or its predecessors developed 40 of the 155 antibiotics ever sold in this country, Kinch said, but is no longer in the antibiotic space. Eli Lilly, AstraZeneca and Bristol-Myers Squibb have also left the antibiotic field, which is now dominated by small companies such as Cubist Pharmaceuticals, formed in 1992 specifically to focus on drugs for resistant bacterial infections that could have higher price points.
His count, Kinch said, if anything, overestimates the number of antibiotics still available, because some of the new drugs are not general-purpose antibiotics. They include, for example, an acne medication and a treatment for anthrax, developed for use in case of a bioterrorist attack.
One reason pharmaceutical companies are withdrawing, Kinch said, is that our patent law squeezes them for time. A patent gives a company 20 years of protection for a new drug, but it takes 11 years of clinical trial experience on average to get a drug approved. That means the typical company has nine years under patent to earn back the development costs before a generic comes in.
If the drug is an antibiotic, there is an additional catch. Because of rising resistance doctors hold new antibiotics in reserve, using them only in cases of dire need. This happened, for example, in the case of vancomycin, which has long been used as a drug of last resort. “When you hold a drug in reserve,” Kinch said, “you’re eating into the patent time a company has to recoup its development costs.”
“If you’ve got this vancomycin-like situation, where the drug is sitting on a shelf—quite literally sitting on a shelf—how is a company going to make its money back? It can’t price the drug at $10,000 a dose.” Companies have consistently decided there is no exit from this trap – as long as we hold to the current model for drug development.
What to do about it?
In the U.S., we’re used to turning to the NIH to solve problems like this, but the NIH budget, which doubled in 2009, has fallen continuously ever since. It is now 30 percent below 2009 levels in constant dollars.
Since the NIH has fallen victim to congressional gridlock, people in the biomedical community are starting to organize on their own. The group Kinch helped found, the Institute for Life Sciences Collaboration, recently convened an expert panel at the United Nations to discuss the need for innovative partnerships and financing models to deal with antibiotic resistance.
One popular idea is “de-linkage,” or finding a way to disconnect the costs of development from the sale of pills. Some have suggested that large prizes, of $1 billion or more, be offered for the development of new drugs, which would then be sold for modest prices by other companies.
The Infectious Diseases Society of America (ISDA) has launched a “10 x 20” initiative whose goal is to create global antibacterial drug research-and-development enterprise with the power in the short-term to develop 10 new, safe and effective antibiotics by 2020.
Britain is offering a prize of £10 million, called the Longitude Prize 2014 (after the prize once offered for an accurate way to determine the longitude of ships at sea), for a rapid test that would allow health professionals to identify bacteria quickly and so administer only the right antibiotics at the right time.
Newly arrived at Washington University in St. Louis, Kinch is just beginning to think about the role the university might play in redefining its role. He points out that the university excels in biomedical research, but is losing brilliant ideas in the Valley of Death between the lab and the market.
Led by Provost and Executive Vice Chancellor H. Holden Thorp, PhD, an enterpreneurship team has been convened to redefine what the university does with biomedical discoveries after the peer-reviewed articles are in print. In addition to Kinch, the team includes Dedric Carter, PhD, associate provost and vice chancellor for entrepreneurship and innovation; and Emre Toker, PhD, managing director of the Skandalaris Center for Entrepreneurial Studies.
One of the university’s assets is School of Medicine research with the human microbiome, the trillions of organisms that live in our guts, many performing beneficial tasks such as digesting food and fighting off infections. Work the microbiome was pioneered by Washington University scientists led by Jeffrey Gordon, MD, the Dr. Robert J. Glaser Distinguished University Professor and director of the Center for Genome Sciences and Systems Biology.
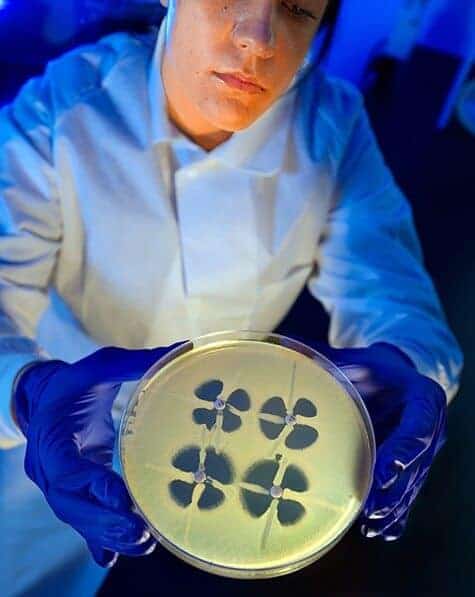
Why is this relevant? In the past the hunting ground for new antibiotics was often the soil. Vancomycin, for example, was found in a soil sample from Borneo. But in the future, the hunting ground may become the natural products produced by the human microbiome. (See “Mining for antibiotics, right under our noses.” )
Antibiotics are not the only drug class heading for trouble—Kinch mentions that HIV/AIDs drugs are following a similar trajectory—but they have become the poster child for the larger problem of drug discovery and development in part because they underpin every part of modern medical practice, from surgery to cancer treatment and pretty much everything in between.


Antibiotic resistance is the scariest thing happening in modern medicine. If we lose antibiotics, we’re going back to the dark ages where people died from infected papercuts.