Anesthesia, long considered a blessing to patients and surgeons, has been a mystery for much of its 160-plus-year history in the operating room.
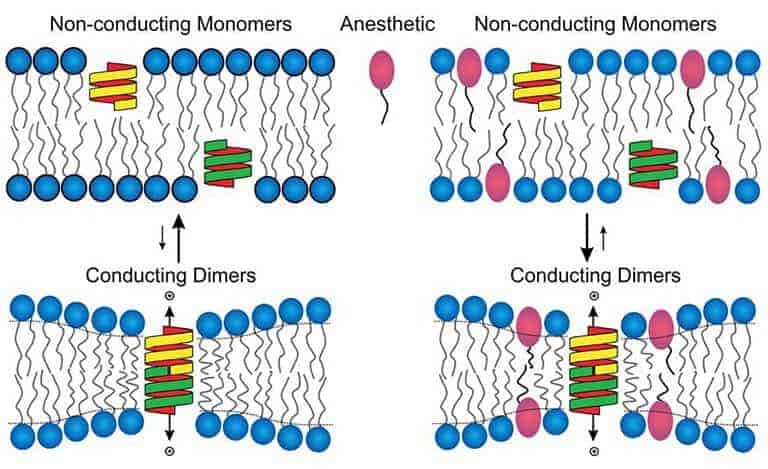
No one could figure out how these drugs interact with the brain to block pain and induce a coma-like, memory-free state. The debate has divided the anesthesia research community into two camps: one that believes anesthetics primarily act on the cell membrane (the lipid bilayer) of nerve cells, perhaps altering it to the point that embedded proteins cannot function normally. The other says the membrane proteins themselves are altered directly by anesthetics.
Now there is new evidence supporting the latter position. A team of researchers from Weill Cornell Medical College has found that it is the proteins that are affected by commonly used anesthesia. Specifically, activity of ion channel proteins that are important for cell-to-cell communication is markedly reduced when anesthetics are applied, the researchers report Nov. 10 in the Journal of General Physiology.
“This is, to our knowledge, the first demonstration that anesthetics alter the function of relevant ion channels without altering properties of the cell membranes,” says the study’s lead investigator, Dr. Hugh C. Hemmings, Jr ., professor and chair of anesthesiology at Weill Cornell, who worked in close collaboration with Dr. Olaf S. Andersen, a lipid bilayer expert and professor of physiology and biophysics at Weill Cornell, who has developed methods to quantify the membrane-perturbing effects of drugs and other molecules.
Importantly, Drs. Hemmings and Andersen note, the studies tested clinically relevant concentrations of isoflurane, a widely used anesthetic. Previous studies that found the membrane was altered used much higher doses of isoflurane — concentrations that would never be used in patients.
The distinction matters, says first author Dr. Karl Herold, a research associate in the Department of Anesthesiology who performed and analyzed the experiments.
“Drugs are not perfect — they always have side effects,” Dr. Herold says.
“You can only improve drugs if you know how they work, which means that you need to know when drugs have non-specific or undesired membrane effects,” Dr. Andersen adds.
“Now that we have a basic understanding of how anesthetics affect cells in the central nervous system, we have knowledge to improve them,” he says. “In the future, we may be able to design anesthetics that do just what we want them to do, and not what we don’t.”