Conventional treatment seeks to eradicate cancer cells by drugs and therapy delivered from outside the cell, which may also affect (and potentially harm) nearby normal cells.
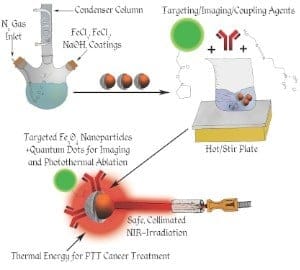
In contrast to conventional cancer therapy, a University of Cincinnati team has developed several novel designs for iron-oxide based nanoparticles that detect, diagnose and destroy cancer cells using photo-thermal therapy (PTT). PTT uses the nanoparticles to focus light-induced heat energy only within the tumor, harming no adjacent normal cells.
The results of the UC work will be presented at the Materials Research Society Conference in Boston Nov. 30-Dec. 5 by Andrew Dunn, doctoral student in materials science engineering in UC’s College of Engineering and Applied Science. Working with Dunn in this study are Donglu Shi, professor of materials science engineering in UC’s College of Engineering and Applied Science; David Mast, associate professor of physics in UC’s McMicken College of Arts and Sciences; and Giovanni Pauletti, associate professor in the James L. Winkle College of Pharmacy.
The UC study used the living cells of mice to successfully test the efficacy of their two-sided nanoparticle designs (one side for cell targeting and the other for treatment delivery) in combination with the PTT. However, the U.S. Food and Drug Administration has now approved the use of iron-oxide nanoparticles in humans. That means the photo-thermal effect of iron-oxide nanoparticles may show, in the next decade, a strong promise in human cancer therapy, likely with localized tumors.
HOW THE NANOPARTICLES WORK WITH PHOTOTHERMAL THERAPY
With this technology, a low-power laser beam is directed at the tumor where a small amount of magnetic iron-oxide nanoparticles are present, either by injecting the particles directly into the tumor or injecting them into the blood stream whereby the particles find and bind to the abnormal cancer cells via cell-specific targeting.
Sufficient heat is then generated locally by the laser light, raising the tumor temperature rapidly to above 43 degrees Celsius, and thereby burning the abnormal cancer cells. This particular PTT treatment does not involve any medicine, but only generates local heat within the tumor, therefore posing much less side effects than the traditional chemo or radiation therapies.
“This treatment is much more ideal because it goes straight to the cancer cell,” says Shi. “The nanomaterials enter only the abnormal cells, illuminating those cells and then doing whatever it is you have designed them to do. In this case, it is to heat up hot enough to burn and kill the cancer cells, but not harm the surrounding normal cells.”
Shi added that physicians are often frustrated with the current conventional means for early imaging of cancer cells through Medical Resonance Imaging or Computerized Tomography scans because the tumors are usually stage three or four before they can be detected. He stated, “With nanomaterial technology, we can detect the tumor early and kill it on sight at the same time.”
CELL TARGETING
- Each tumor has a corresponding protein that is cancer specific called a tumor specific ligand or an antibody antigen reaction that only has expression for that specific cancer such as breast or prostate cancer.
- Scientists identify this certain bio-marker that is specific to a certain tumor, then conjugates this bio-marker on the surface of the nanocarrier that only has the expression for that specific kind of cancer cell.
- It then only targets the abnormal cancer cell, not normal, healthy cells, and because it is so small it can break the membrane and enter that conjugated cancer cell and release the PTT.
- The nanotech carriers go into the body through a vein in the blood stream, seek the abnormal cancer cells, find the bio-marker or cancer cells and attach to those cells and unlock their florescent particles so they can be detected by a photon laser-light.
- The laser-light heats the nanoparticles to at least 43 degrees Celsius to kill the cancer cells, ultimately leaving all the other cells in the body unharmed.
POTENTIAL DIY CANCER TREATMENT
The procedure can ultimately be carried out by the patient themselves after being trained how to direct a small laser light device to the affected area for a specified amount of time two to three times a day. This method can ultimately improve the success rate, as well as cut costs to the patient. This gives “point and shoot” a whole new meaning.
FUTURE RESEARCH DIRECTION
Future research in nanoparticle PTT will look at toxicity, biodegradability and compatibility issues. Shi said that the team is currently looking for other diverse biodegradable materials to use for the carriers such as plant chlorophylls like those in cabbage that are both edible and photothermal. This material is biocompatible and biodegradable and can potentially stay in the tumor cells until its job is finished, then dissolve and be passed out through the digestive system.
Support for this research was provided by a National Science Foundation grant under contract number MSF (1343568) titled “Development of Nanotechnology Minor Focused on Nano Biomedicine and Sustainable Energy.” For more information, please visit Shi’s website at:
http://homepages.uc.edu/~shid/