Blood research conducted by biomedical engineers from The University of Texas at San Antonio (UTSA) College of Engineering, in collaboration with the Blood Research Program of the U.S. Army Institute of Surgical Research(USAISR), could change the way injured soldiers are treated on the battlefield.
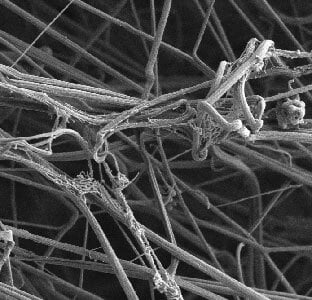
In battlefield settings, stopping a patient’s bleeding is integral to successful treatment. Platelets are blood cells that are integral to the body’s natural clotting procedures, which assist in stopping bleeding. During surgery, platelets are transfused when a patient has lost massive amounts of blood due to injuries.
In collaboration with the USAISR, Anand Ramasubramanian, associate professor in the UTSA Department of Biomedical Engineering and the South Texas Center for Emerging Infectious Diseases, and his team of UTSA graduate students subjected platelets stored in refrigerated temperatures to a battery of tests. For the past five years, Ramasubramanian and his graduate students have been closely working with Lt. Colonel (LTC) Andrew Cap, chief of Coagulation and Blood Research and his team at USAISR.
These researchers found that cold-stored platelets could actually be a more effective alternative in the cessation of bleeding than the current standard-of-care product. Results from the laboratory showed that cold-stored platelets not only respond better to injuries and form stronger clots but also are safe. For battlefield surgery purposes, these findings could be the difference between life and death for many injured soldiers.
In most transfusion procedures, medical professionals obtain platelets from blood banks where the platelets are stored in bags at room temperature. However, room temperature platelets are only approved for use for a maximum of five days. They are then discarded. In battlefield conditions, where resources are scarce, storing platelets for longer periods than that is vital.
“In the cold, the metabolism of the platelets are slowed down so that they retain their energy reserves to such an extent that they are still effective even after five days in storage,” said Ramasubramanian. “In fact, some of our results have shown promise that you may be able to store for up to two weeks. And remember, two weeks is a sufficiently long time to help with transportation logistics.”
Recently, a team of doctors in Norway successfully transfused cold-stored platelet into a patient undergoing reparative surgery for a tear in the inner wall of the aorta, the main artery of the human body. The transfusion demonstrated the UTSA and the USAISR’s concept of using cold stored platelets as a viable alternative to the current standard of care.
According to Heather Pidcoke, research physiologist at USAISR and one of the lead researchers on this project, the patient showed significant improvement in their condition immediately after surgery, compared patients who have undergone similar procedures in the past with standard-of-care product.
“The surgical success of our Norwegian colleagues and collaborators is a key milestone in the evaluation of cold-stored platelets,” said LTC Cap. “This breakthrough in blood research is of historic significance for not only our research collaborators but to the medical community as a whole.”
“This success story is an example of what great partnerships can accomplish,” said Ramasubramanian. “I should also add that we could not have accomplished this without the motivated graduate students who drove the project forward.” BME graduate students Robbie Montgomery, Kristin Reddoch and Prajeeda Nairparticipated in this project. Montgomery is now a senior biomedical technician at USAISR.
Over the next several years, the UTSA and USAISR researchers will test the limitations and clinical safety of future cold platelet transfusions to better understand how military and civilian medical professionals can successfully leverage them.