Genetic research suggests that hundreds of genes are likely risk factors for neurodevelopmental disorders such as autism. This heterogeneity presents both challenges and opportunities when it comes to developing effective treatments for these diseases. The next generation of research must focus on the neural circuits underlying behavioral symptoms, the cell types in these circuits, and the signaling pathways that connect the diverse genes that potentially cause disease.
In a new paper in the journal Science, Mriganka Sur, professor at the Picower Institute for Learning and Memory and MIT Department of Brain and Cognitive Sciences, and Mustafa Sahin of Boston Children’s Hospital explain why leveraging the heterogeneity observed in autism spectrum disorder (ASD) will empower scientists to develop the precision therapies required to successfully treat the disease and others like it.
Embracing diversity to nurture precision
“Heterogeneity has been a huge obstacle in ASD research,” Sur, the Newton Professor of Neuroscience and director of the Simons Center for the Social Brain, says. “But scientists are starting to take advantage of the broad range of behavioral symptoms and degrees of impairment that are characteristic of the disorder.” Researchers are expanding their investigations beyond “pure autism” (no intellectual disability) to examine related genetic disorders such as Fragile X and Rett syndrome. They are also looking at the individual genomes and environmental interactions of individuals diagnosed with autism. These combined efforts are expected to enhance understanding of the underlying clusters of symptoms specifically associated with ASD, which, in turn, will drive the development of more effective treatments.
ASD is a complex disorder. Given the large number of genes potentially responsible for autism, it is impossible to develop a one-size-fits-all treatment. On the other hand, it is also unrealistic to expect specific interventions for every genetic cause. It makes sense to focus on a few molecular and circuit pathways that can be targeted by a limited number of mechanism-based treatments. Current efforts are concentrating on single-gene mutations that reveal a prevalence of ASD symptoms.
Designing successful clinical trials
Sur and Sahin discuss obstacles faced in current research initiatives and propose recommendations for future clinical trials designed to deliver precision medicine. Challenges include selecting the right group of patients, defining the optimal duration for the trial, ensuring that drugs engage their targets, and optimizing animal models to ensure direct relevance for human outcomes.
Translatable biomarkers that can be employed in both mouse models and human subjects are particularly powerful, according to the paper’s co-authors. A critical feature of precision clinical trial design, these biomarkers can effectively predict subjects most likely to respond, confirm target engagement, and detect early signs of efficacy. A panel of significant biomarkers that provides a unique profile of a patient will allow scientists to interrogate the most relevant ASD-related circuits, which can assist in early diagnosis and assessing phonotype and severity. The critical age window for treatment of autism remains unclear, but there is no doubt that biomarkers will be important for ensuring effectiveness.
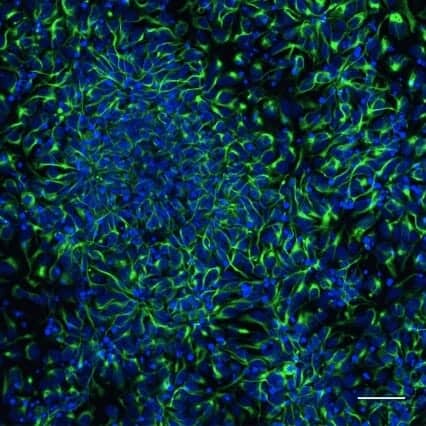
Sur and Sahin include two additional suggestions for clinical trials. They recommend using available technology to observe the effects of test drugs on a patient’s neurons before directly administering a pharmaceutical therapy. They also caution researchers exploring gene therapy to carefully regulate dosage levels since elevated expression of particular genes can have harmful effects. They predict that those who conduct trials based on a mechanistic understanding of autism performed on a well-defined group of subjects with evidence of target engagement and supportive biomarkers are the most likely to succeed.
Treatment ramifications and challenges
Today, two FDA-approved drugs are used to treat autism, and both are aimed at relieving irritability rather than the core manifestations of the disorder. Since single-gene conditions involve multiple potential targets, combination rather than singular drug therapies will likely be most effective. Also, while drug therapies may normalize neuronal abnormalities, cognitive function depends on complex circuits and an individual’s interaction with the environment. Thus, a drug therapy may correct synaptic abnormality, and even accelerate the rate of learning, but it may not result in behavioral changes. A combination of behavioral and pharmacological interventions appears to comprise the most promising treatment approaches.
Yet even if neuroscientists are successful in enhancing their understanding of single-gene syndromes that cause autism, roadblocks will remain. A comparative analysis of the various genetic causes of ASD will be required to determine if treatment for one may be effective for another. At the same time, there is still no way to classify patients according to genetic, biochemical or circuit abnormalities, and no analytical tool exists to determine if someone with ASD would benefit from an effective treatment.
However, given that autism affects 1 in 68 children and exacts an annual toll of approximately $35 billion in the U.S. alone according to the Centers for Disease Control, scientists are committed to overcoming these obstacles and delivering precision medicine for ASD and related neurodegenerative disorders.