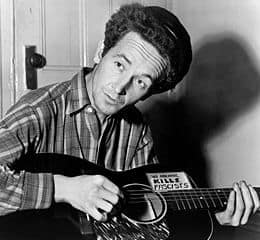
Perhaps the most famous name associated with Huntington’s disease is that of populist folk singer Woody Guthrie, who died of it at age 52 in 1967. Guthrie’s mom had died of it, too, when Woody was a teenager. So, it’s believed, did his mom’s dad. Two of Woody’s children by his first wife, Mary, died at age 41 of Huntington’s. (In 1968, his second wife, Marjorie, founded the Huntington’s Disease Society of America.)
A person first diagnosed with Huntington’s disease, an ultimately lethal genetic neurodegenerative disorder characterized by jerky movement as well as cognitive and psychiatric problems, can on average expect to live another 20 years – but not without heartache. There are drugs to alleviate some symptoms of Huntington’s, which most often manifests in the fourth and fifth decades of life, but none that delay its onset or slow its progression.
Work by Stanford neuroscientist Frank Longo, MD, PhD, may change that. As described in a study just published in The Journal of Neuroscience, Longo and his colleagues have shown that a drug that mimics some aspects of a key brain protein was able to reduce degeneration and movement deficits associated with Huntington’s disease in two different mouse models of the disorder. The findings add to a growing body of evidence that protecting or boosting neurotrophins — bulky proteinaceous molecules that support the survival and function of nerve cells — may slow the progression of Huntington’s disease and other neurodegenerative conditions.
Longo’s team used a compound called LM22A-4, unearthed by Longo a couple of years ago in a computer search in collaboration with University of California-San Francisco neurologist Steven Massa, MD, PhD. LM22A-4 is a small molecule with less than 1/70 the bulk of the particular protein it mimics: brain-derived neurotrophic factor or BDNF, which has been studied in depth by many researchers and is known to be critical during the development of the nervous system and involved in important brain functions including memory and learning.
But unlike BDNF, LM22A-4 binds to and activates only one of two major cell-surface receptors for BDNF found in nerve cells. That’s a good thing, because the receptor LM22A-4 activates is associated with BDNF’s long-known ability to foster the survival of newborn nerve cells, while the receptor it doesn’t activate has been shown to respond to BDNF stimulation by inducing the death of nerve cells. This is helpful, perhaps, during early development when the brain needs to prune redundant nerve circuitry produced in a series of growth spurts, but it’s presumably going to be counterproductive in the treatment of a neuron-destroying disorder like Huntington’s.
Longo’s group examined the effects of LM22A-4 treatment in mice that were predisposed to develop symptoms of Huntington’s disease rapidly (within weeks) or gradually (within months). LM22A-4 treatment reduced the accumulation of abnormal proteins in the striatum and cortex — brain regions affected in Huntington’s disease. Motor behaviors (downward climbing and grip strength) also improved in the mice that received daily LM22A-4 treatments.
LM22A-4 has also shown promise in the treatment of stroke and other brain conditions. Because it was already commercially available when Longo and his colleagues’ computer stumbled on it, it also promises to be relatively cheap – kind of a “folk drug” – should any of its potential applications pan out. That would make Woody proud.