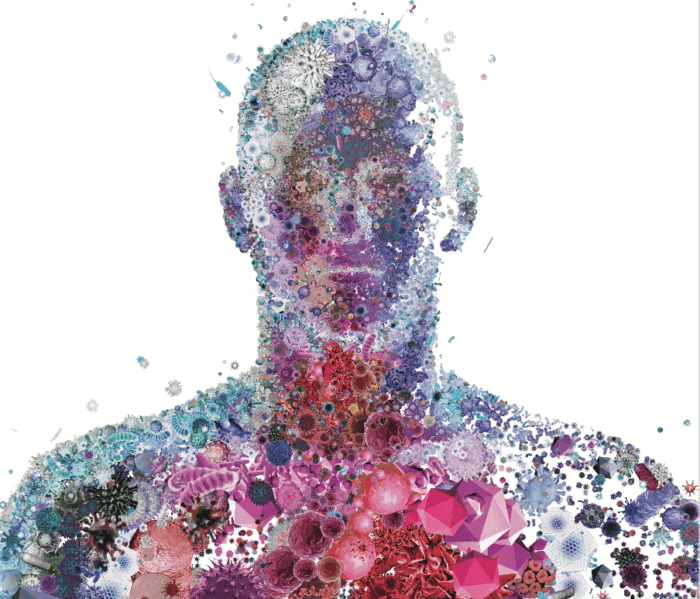
Just as we’re getting used to knowing we have trillions of bacteria populating us, from our eyeballs to our intestines, comes word that we need to look beyond bacteria to even smaller squatters: the virome, a vast community of viruses that calls us home.
Some of your viruses are just visiting and will be gone in a week. Most are permanent tenants. A few may even find their way into your DNA. In fact, we—along with most other mammals—owe our very existence to viruses that took up residence in the chromosomes of distant ancestors millions of years ago. Because of those embedded viral genes, animals evolved that make a placenta, the organ that supports the developing fetus during gestation.
“Most mammals are characterized by the fact that we bear live young that were nourished by a placenta,” says Penn State biologist Peter Hudson. “We would not be who we are if it wasn’t for the fact that we have virus DNA within our DNA.”
The viruses most on Hudson’s mind these days are not so helpful. They have names like Zika, Chikungunya, SARS, H5N1, and they have suddenly jumped from the animals they normally infect—apes, birds, bats, mice—to cause epidemics in human populations.
“We’re talking about diseases that we can’t control, and diseases we did not know were a threat to humans,” says Hudson.
“Most of the emerging infectious diseases that arise come from wildlife reservoir hosts,” says research associate Kurt Vandegrift, who did his doctoral work in Hudson’s lab and now runs a research program of his own. “When we find a new one, there’s always a scramble to find out where it came from. What species is the reservoir host? How did the virus get into humans? How does it spread? We never know this information, we don’t have a vaccine, we don’t have any of these things. We’re really behind the 8-ball.”
Hudson and Vandegrift aren’t virologists or medical doctors. They’re wildlife biologists in the classical mold, trained to observe animals in their natural habitat. They think one key to fighting emerging diseases is finding out before they get into humans which pathogens we’re mostly likely to encounter—the ones that are carried by the wild creatures we’re most likely to touch, share space with, or be bitten by. For people who live in the eastern U.S., the list of “peri-domestic” species includes deer, rabbits, chipmunks, and the white-footed mouse, as well as the ticks and mosquitoes that feed on both our furry neighbors and ourselves.
Aside from bug bites, we pick up viruses from these creatures through contact—removing a mouse from a trap, handling game during a hunting trip—or by inhaling their dust and dander in cupboards, sheds, and other confined places. As Vandegrift memorably puts it, “We breathe their fecal by-products.”
In 2012 Vandegrift and Hudson launched a study of the community ecology of the white-footed mouse: How many are there, what makes their numbers go up and down, what’s their social structure, what parasites do they have, and how do the parasites spread through the population?
“We need to understand the dynamics of the mouse population,” says Hudson. “As they increase, so the risk of infection to us increases—there’s more mice, there’s more ticks, there’s more disease transmission taking place.”
The implications of the study reach beyond mice and the diseases they carry, says Vandegrift. “We’re using a wildlife system to learn how we can monitor and manipulate things, to then inform public health practices in humans. Or at least give us an idea about what we should look for.”
To catch a mouse
Their target animal was easy to find. The white-footed mouse, Peromyscus leucopus (PAIR-oh-MIS-kus loo-KOH-pus), ranges throughout most of the eastern two-thirds of the U.S. and is abundant in and around Penn State’s University Park campus.
“They’re everywhere,” says Vandegrift. “They’re so adaptable.” They live in houses, barns, and sheds, under tent platforms and in woodpiles, in long-parked cars and lawnmowers. They also carry several pathogens that can infect humans, such as Borrelia, the bacterium that causes Lyme disease, and the hantavirus, which kills nearly 40 percent of the people it infects. “I don’t touch any of these critters without wearing gloves,” says Vandegrift. “The hantavirus seriously freaks me out. It’s only in extreme cases that people get it—but we are an extreme case, seeking out these animals and spending eight hours a day around them.”
Three times a week, he and his team of graduate and undergraduate students set out live traps baited with oats in two dozen 100-meter-square grids on a wooded hillside southwest of town. Each caught mouse gets the equivalent of a thorough medical exam: The researchers weigh and measure it, estimate its age, check its overall condition, whether it has bred recently and how many fleas and ticks it carries, and gather blood and fecal samples for analysis in the lab. It also gets a tiny Passive Induced Transponder (PIT) tag inserted into the scruff to trace its movements and range. Like a pet’s microchip, the tag provides a unique ID number that can be read by an electronic scanner. If a trapped mouse already has a tag, the team scans it and records the information from it before releasing the mouse to carry on with its life.
“We can actually follow individuals through time,” says Vandegrift. “We know who lives where and whose home ranges overlap or touch. We can check whether they have been exposed to a certain pathogen, and we can know when they got infected. Ideally, we should be able to watch parasites flow through the populations.”
An unusual corporate partnership
Vandegrift found that Peromyscus numbers in his study area vary widely; sometimes a sampling grid yields one mouse per day, other times it catches 100. But he learned from colleagues doing similar trapping studies that the population highs and lows near State College do not match the highs and lows elsewhere in the region over the same period. That lack of synchrony makes it much harder to correlate population levels with disease transmission.
Figuring out the population cycles of a wild species by doing a trapping study is incredibly laborious in one small location. To do it over the entire country, or even just the Northeast, is simply not feasible.
Trying to come up with a way of estimating mouse population cycles, Vandegrift recalled the classic example of Canada lynx and snowshoe hares, a roughly 10-year wax-wane cycle between predator and prey. To discover that cycle experimentally would have meant catching and counting lynx and hares, year-round, for decades.
As it happens, the lynx-hare cycle was not found by doing field work. It was discovered by studying the fur-trapping records of the Hudson’s Bay Company from the 1820s into the early 1900s. Trappers turned in more hare and lynx pelts in years of abundance of each species, and fewer in years of scarcity. In that nearly century-long record, the 10-year cycles were clear.
Vandegrift wondered whether comparable records were available that would be relevant to Peromyscus numbers.
“We thought and we thought,” says Vandegrift. “And we thought, maybe it’s mousetrap sales, because people don’t buy mousetraps unless they see a mouse in the house, and that happens primarily when the populations are elevated.”
He contacted Woodstream, Inc., the company that makes Victor mousetraps, and asked if they would share their sales figures with him. The Woodstream people sent records for the past 10 years broken down by postal code, by week, for all of the U.S., Puerto Rico, and Canada. “It’s a huge file—a HUGE file—more data than I’ve ever dealt with,” says Vandegrift.
His lab is now comparing that data with results of other trapping studies done in the same time frame across the US, to see if mousetrap sales are indeed a reliable indicator of mouse population numbers. If they are, Vandegrift can use the sales figures to construct long-term Peromyscus population maps for any area of concern. So far, it’s looking good.
Going viral
Seed money from Hudson’s Willaman Chair endowment enabled Vandegrift to start the field studies, but at the time, tests to identify viruses were prohibitively expensive. Without the means to catalog the entire community of viruses the mice carry, he checked the blood samples for a few viral infections for which tests were available. He also checked for gut worms, parasites large enough to be identified with a relatively low-cost, low-power microscope. He encountered one kind of worm he had to send to an expert for identification. It turned out to be a new species, which has since been named after him—Heligmosomoides vandegrifti. “I told my mother that now I don’t have to have children, because I’ve preserved the family name forever,” he says.
Then, as word of his fieldwork got around, a group of Columbia University scientists led by Amit Kapoor, now at Nationwide Children’s Hospital in Columbus, Ohio, got in touch with Vandegrift to ask if they could have blood samples from his mice. They wanted to test for a virus similar to Hepatitis C, in hopes that Peromyscus could serve as a model system for studying the disease.
According to the Centers for Disease Control, close to 200 million people worldwide carry Hep C as a chronic infection, and about 20,000 Americans die from it each year. The Hep C virus has been notoriously hard to study because other than humans, it was known to infect only chimps and horses, neither of which anyone wanted to experiment on. Finding a version of Hep C in Peromyscus, which is easy to handle in a laboratory, could greatly improve the odds of developing treatments or possibly even a vaccine for the disease.
Vandegrift agreed to his colleagues’ request, and added one of his own. “Could you identify all the viruses in the samples? Because we have this data set on the population biology that nobody else has, and we could really make use of those,” he recalls. “And they said OK.”
With powerful and less costly new “454” DNA-sequencing technology, the Columbia team compared all the potential viral DNA in the mouse samples with the DNA sequences in GenBank, a massive library compiled from thousands of species. The result was the first comprehensive study of the Peromyscus virome.
The Peromyscus samples do not have any of the viruses typically seen in lab mice—“They’re a different species, so you shouldn’t really expect that,” he says—but they do have at least eight that had never been identified before, including a form of Hepatitis C. Vandegrift and his lab are now studying the course of the disease in Peromyscus. Humans don’t catch the mouse version of the virus, but if the illness it causes in Peromyscus is similar to what happens in people, the adaptable little mouse could become a great boon to those researching the human form of the disease.
Keeping it real
The Peromyscus virome project was so successful that Vandegrift, Hudson, Kapoor and other colleagues have gone on to survey the virome of the deer tick (Ixodes scapularis, also known as the black-legged tick). The project has the potential to spot viruses that don’t currently pose a threat to humans but that could jump to us if they undergo a small genetic change that allows them to infect people or makes them more virulent. Like finding the relative of Hep C in mice, such a discovery would let us study how the virus works and how it is transmitted. “We could even create a vaccine for it pre-emptively, so if it does spill over into humans, we’re finally not behind the 8-ball,” says Vandegrift.
The research team recently won a $2.35 million grant from the National Science Foundation to study the complex interactions between Peromyscus and its viruses, including how they relate to each other during an infection and over time. This goes far beyond an inventory of the viruses the mice carry. It’s more like a detailed community history, and it could help solve one of the persistent mysteries of medicine: Why do some people get much sicker than others with the same illness?
Genetics has something to do with it, but Hudson and Vandegrift think it has more to do with the fact that we are rarely, if ever, infected by just one germ at a time—and since pathogens change your immune system, how sick you get from a new pathogen doesn’t depend only on the ones you’re infected with now; it’s a reflection of all the infectious diseases you’ve ever had, and even in what order you had them.
“Your ability to be invaded depends on what’s happened in your life,” Hudson says. “It’s going to be different for everybody, because everybody’s life is different.”
He offers himself—a native of Great Britain who has worked with wildlife in Africa, Australia, and the Americas—as an example. “I have had tuberculosis, I’ve had sleeping sickness. I was also infected with measles, chicken pox, rubella, German measles, all of those childhood diseases. Given that, what is my susceptibility to new infections? Am I less likely or more likely to get malaria or to get Chikungunya or to get Zika virus?”
The new project, again working with the wild mice of central Pennsylvania, will help them understand those kinds of interactions in a way no lab study ever could.
“We always consider parasites in isolation, but they almost never exist in isolation,” says Vandegrift. “The dynamics of that pathogen may be totally different if the host has another infection. Studying it in a wild population gives us all of these biological realities that you don’t have in a lab.
“It’s real science. Real complicated, though.”