Why do some people with cold sores around their lips experience painful lesions, while others have no symptoms at all, yet still spread the virus? A new study conducted at Penn State finds that these differences could be due to variations in the way certain strains of herpes simplex (HSV-1) — the virus that causes cold sores, as well as genital herpes — activate gene expression in neurons.
“HSV-1 occurs in more than half the global population,” said Moriah Szpara, associate professor of biology and biochemistry and molecular biology. “Not only does it cause recurrent problems, such as cold sores and genital herpes, but recent research has implicated chronic HSV-1 infection with the development of disease later in life, including neurodegenerative diseases like Alzheimer’s.”
Szpara explained that the HSV-1 lifecycle begins upon contact with mucosal surfaces, where it invades skin cells, replicates, and can induce local lesion formation. The virus also enters local nerve endings in the skin, and transits into neurons in the nervous system. There the virus can lie dormant until it reactivates on future occasions. Neuronal damage and host immune responses triggered by viral reactivations are thought to contribute to long-term neurodegeneration.
“Since every person carries a subtly different version of HSV-1, this might explain some of the variation in human responses to infection; for example, why people have different triggers for their outbreaks or why some people experience more painful sores. Differences in the frequency of viral outbreaks, or in virus-induced gene expression patterns, might also affect the different rates at which people with chronic infections go on to develop neurodegenerative diseases.”
To investigate the causes of this variation in responses, Szpara and her colleagues infected human neuronal cells with one of three HSV-1 strains that are known to differ in their ability to cause disease in the nervous system. Next, they used deep sequencing to identify and quantify the transcriptomes — the entire set of messenger RNAs (mRNAs) made in a cell at any given time — of the neurons during infection by HSV-1.
According to Szpara, when a neuronal cell is infected with HSV-1, the resulting transcriptome includes the whole collection of mRNAs produced by both the human neuron and the HSV-1 virus. By looking at the timing and amount of mRNAs expressed during infection, scientists can gain insights on the proteins that will soon be produced from those mRNAs. It is the viral proteins and new viral progeny produced during infection that ultimately lead to health problems.
“By simultaneously examining both the viral and neuronal transcriptomes in the infected cells we were able to observe the interplay between the timing of viral mRNA production and protein production, and the ensuing host responses,” said Szpara.
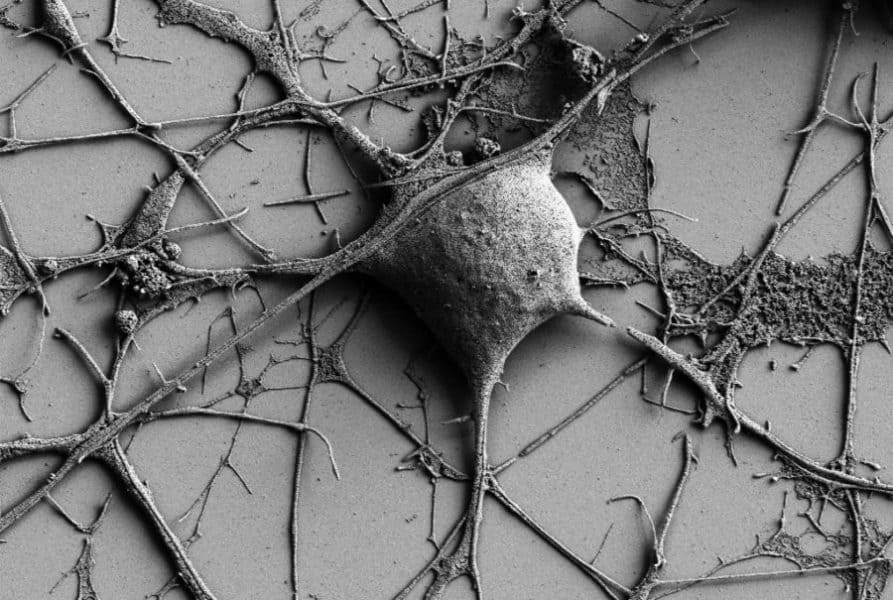
The scientists used two additional techniques — immunofluorescence staining of neurons and Western blotting for viral protein levels — to observe the outcomes of viral and host gene expression. They also used scanning electron microscopy to directly observe changes in neuronal morphology during infection.
Their findings appeared online in PLOS Pathogens on March 22.
The researchers found that different genetic variants of HSV-1 induce different patterns of gene expression in human neuronal cells. Specifically, they found that the viral variants expressed their genes at different rates and quantities, which likely contributes to the different timing and severity of symptoms within hosts. For example, they discovered that one of the variants, which exhibits lower virulence in animal models, displays a different and seemingly delayed pace of viral and host gene expression in neurons. In another example, they found that one variant caused greater changes in expression of genes involved in cell adhesion (or ability of cells to attach to each other), which could impact cell-to-cell spread of HSV-1.
The team also found that these different patterns of gene expression were dependent on the whether the infected cell was a neuron or a skin cell type.
“Together, these data demonstrate the importance of studying virus strain- and cell-type-specific factors that may contribute to neurovirulence in vivo. It also highlights the specificity of HSV-1–host interactions,” said Szpara. “Our study suggests that differences observed between viral variants in cell-based models like neurons can be used to help understand the more-complex interactions of viruses with hosts.”
Other authors on the paper include Colleen Mangold, postdoctoral scholar in entomology; Molly Rathbun, graduate student in biochemistry and molecular biology; Daniel Renner, computational scientist in the Huck Institutes of the Life Sciences; and Chad Kuny, assistant research professor of biology.
This research was supported by Penn State, the Pennsylvania Department of Health, the American Heart Association and the National Institutes of Health.