Chronic wounds are a major health problem for diabetic patients and the elderly – in extreme cases they can even lead to amputation. Using electric stimulation, researchers in a project at Chalmers University of Technology, Sweden, and the University of Freiburg, Germany, have developed a method that speeds up the healing process, making wounds heal three times faster.
There is an old Swedish saying that one should never neglect a small wound or a friend in need. For most people, a small wound does not lead to any serious complications, but many common diagnoses make wound healing far more difficult. People with diabetes, spinal injuries or poor blood circulation have impaired wound healing ability. This means a greater risk of infection and chronic wounds – which in the long run can lead to such serious consequences as amputation.
Now a group of researchers at Chalmers and the University of Freiburg have developed a method using electric stimulation to speed up the healing process.
“Chronic wounds are a huge societal problem that we don’t hear a lot about. Our discovery of a method that may heal wounds up to three times faster can be a game changer for diabetic and elderly people, among others, who often suffer greatly from wounds that won’t heal,” says Maria Asplund, Associate Professor of Bioelectronics at Chalmers University of Technology and head of research on the project.
Electric guidance of cells for faster healing
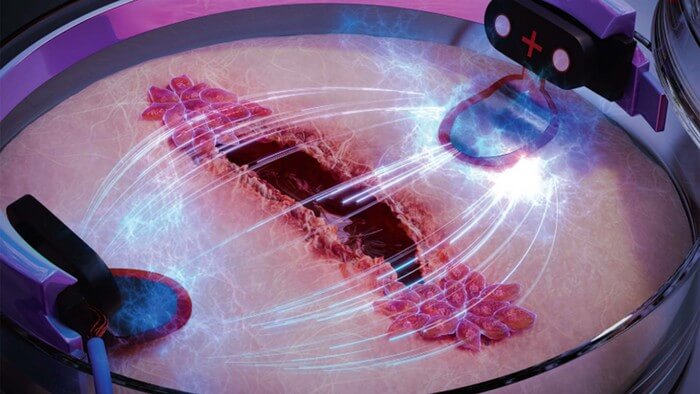
The researchers worked from an old hypothesis that electric stimulation of damaged skin can be used to heal wounds. The idea is that skin cells are electrotactic, which means that they directionally ‘migrate’ in electric fields. This means that if an electric field is placed in a petri dish with skin cells, the cells stop moving randomly and start moving in the same direction. The researchers investigated how this principle can be used to electrically guide the cells in order to make wounds heal faster. Using a tiny engineered chip, the researchers were able to compare wound healing in artificial skin, stimulating one wound with electricity and letting one heal without electricity. The differences were striking.
“We were able to show that the old hypothesis about electric stimulation can be used to make wounds heal significantly faster. In order to study exactly how this works for wounds, we developed a kind of biochip on which we cultured skin cells, which we then made tiny wounds in. Then we stimulated one wound with an electric field, which clearly led to it healing three times as fast as the wound that healed without electric stimulation,” Maria Asplund says.
Hope for diabetes patients
In the study, the researchers also focused on wound healing in connection with diabetes, a growing health problem worldwide. One in 11 adults today has some form of diabetes according to the World Health Organization (WHO) and the International Diabetes Federation.
“We’ve looked at diabetes models of wounds and investigated whether our method could be effective even in those cases. We saw that when we mimic diabetes in the cells, the wounds on the chip heal very slowly. However, with electric stimulation we can increase the speed of healing so that the diabetes-affected cells almost correspond to healthy skin cells,” Asplund says.
Individualised treatment the next step
The Chalmers researchers recently received a large grant which will allow them to continue their research in the field, and in the long run enable the development of wound healing products for consumers on the market. Similar products have come out before, but more basic research is required to develop effective products that generate enough electric field strength and stimulate in the right way for each individual. This is where Asplund and her colleagues come into the picture:
“We are now looking at how different skin cells interact during stimulation, to take a step closer to a realistic wound. We want to develop a concept to be able to ‘scan’ wounds and adapt the stimulation based on the individual wound. We are convinced that this is the key to effectively helping individuals with slow-healing wounds in the future,” Asplund says.
More about the study:
- “Bioelectronic microfluidic wound healing: a platform for investigating direct current stimulation of injured cell collectives” was published in the journal Lab on a Chip. The article was written by Sebastian Shaner, Anna Savelyeva, Anja Kvartuh, Nicole Jedrusik, Lukas Matter, José Leal and Maria Asplund. The researchers work at the University of Freiburg in Germany and Chalmers University of Technology.
- In their study, the researchers showed that wound healing on artificial skin stimulated with electric current was three times faster than on the skin that healed naturally. The electric field was low, about 200 mV/mm, and did not have a negative impact on the cells.
- The method the researchers developed is based on a microfluidic biochip on which artificial skin can be grown, stimulated with an electric current and studied in an effective and controlled manner. The concept allows researchers to conduct multiple experiments in parallel on the same chip.
- The research project began in 2018 and is funded by the European Research Council (ERC). The project was recently granted more funding so the research can get one step closer to the market and the benefit of patients.
For more information, please contact:
Maria Asplund, Associate Professor of Bioelectronics, Department of Microtechnology and Nanoscience at Chalmers University of Technology, Sweden
[email protected] +46 31 772 41 14
Sebastian Shaner, PhD Candidate, Department of Microsystems Engineering at the University of Freiburg, Germany [email protected]