Editor’s note: During the culture wars spurred by the COVID 19 pandemic, it often occurred to us that if the infection led to rapid-onset blindness of many, rather than the death of primarily the elderly and vulnerable, debates over vaccination and masking would have been radically different.
New research reveals that SARS-CoV-2 infection can damage cells crucial for maintaining healthy vision, with potential long-term implications for age-related eye diseases. The study shows how the virus specifically targets and disrupts the function of retinal cells that support the eye’s light-sensing photoreceptors.
Published in PNAS Nexus | Estimated reading time: 4 minutes
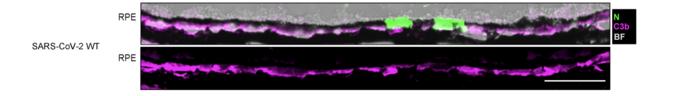
Using both mouse models and human cell cultures, researchers at the University of California, Los Angeles led by Nan Hultgren and David Williams have uncovered how SARS-CoV-2 can infect and damage the retinal pigment epithelium (RPE), a critical layer of cells that maintains vision by supporting photoreceptors in the eye.
The findings suggest that COVID-19 infection could accelerate the onset and progression of age-related macular degeneration (AMD), the leading cause of vision impairment in industrialized nations. “SARS-CoV-2 infection appears to induce a proinflammatory response in the RPE cells that involves complement activation and increased production and secretion of inflammatory cytokines,” explains Hultgren.
The research team discovered that the virus can reach the RPE cells through multiple routes and cause widespread inflammation across the retinal layer, even when only a few cells show active infection. Most concerning was the virus’s ability to impair key RPE functions – including the maintenance of a critical blood-retina barrier and the recycling of photoreceptor components essential for vision.
Of particular significance was the finding that different COVID-19 variants displayed varying levels of damage. While the original strain caused more immediate inflammation, the Omicron variant showed a delayed but more prolonged inflammatory response that could have more serious long-term consequences.
The researchers also identified specific viral proteins that disrupted normal RPE cell function. Their experiments revealed that even individual SARS-CoV-2 proteins could cause cellular changes that made the RPE more vulnerable to stress and damage – effects that parallel early stages of macular degeneration.
Glossary
- Retinal Pigment Epithelium (RPE)
- A layer of cells in the retina that nourishes visual cells and is essential for maintaining healthy vision.
- Age-Related Macular Degeneration (AMD)
- A leading cause of vision loss that occurs when the central portion of the retina, called the macula, deteriorates.
- Complement Activation
- Part of the immune response that helps fight infection but can also contribute to tissue damage when overactive.
Test Your Knowledge
What is the main function of the retinal pigment epithelium (RPE)?
The RPE maintains vision by supporting and nourishing the eye’s photoreceptors and maintaining the blood-retina barrier.
How can SARS-CoV-2 affect RPE cells?
The virus can damage RPE cells by triggering inflammation, disrupting their barrier function, and impairing their ability to recycle photoreceptor components.
How do the effects of different COVID-19 variants on RPE cells compare?
While the original strain caused more immediate inflammation, the Omicron variant induced a delayed but more prolonged inflammatory response that could have greater long-term impact.
What is the potential connection between COVID-19 infection and age-related macular degeneration?
The inflammatory responses and cellular changes caused by SARS-CoV-2 infection parallel those seen in early AMD, suggesting that infection could accelerate the onset and progression of this eye disease.
Enjoy this story? Subscribe to our newsletter at scienceblog.substack.com.