Researchers from Massachusetts General Hospital say they’ve made an important step towards greater availability of hand transplants, face transplants and other transplants involving multiple types of tissue.
In their report in the American Journal of Transplantation, the team describes how a procedure developed at the MGH to induce immune tolerance to organ transplants also induces tolerance to a model limb transplant in miniature swine. Transplantation of donor bone marrow – either several months before or simultaneous with the transplant – allowed the animals to accept what are called vascularized composite allografts (VCAs) from immunologically mismatched donors.
“The need for lifelong immunosuppression to prevent graft rejection is the most important challenge in this type of procedure, since most potential VCA recipients are young and would face increased risks of infection, diabetes or kidney problems, and even some types of cancer over many years,” says Curtis L. Cetrulo, Jr., MD, head of the Hand Transplantation Service in the MGH Division of Plastic and Reconstructive Surgery and senior author of the current report.
“Bringing immunologic tolerance to hand and face transplantation would result in a paradigm shift in the way we will be able to treat the horrific injuries our service members are sustaining in the current military conflicts in Iraq and Afghanistan, as well for the types of blast-injury extremity loss seen in the Boston Marathon bombing. Tolerance would give us a unique tool – a real game changer – with which to help these patients,” he says.
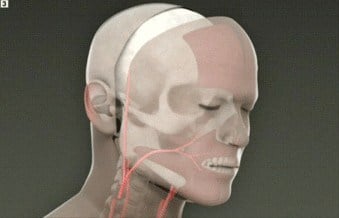
Most frequently used to replace amputated hands and arms and to repair severe facial injuries, VCAs involve transplantation of muscle, bone, skin and nerves. While offering significant improvement in recipients’ quality of life, the procedures are not required to preserve a patient’s life, making the need for lifelong immunosuppression a disadvantage. The induction of immune tolerance – essentially tricking a recipient’s immune system into accepting donor tissue – could be an ideal solution to that problem.
The MGH is a world leader in the development of tolerance-inducing protocols. Several decades of research led by David H. Sachs, MD, founder and scientific director of the MGH Transplantation Biology Research Center (TBRC), led to a protocol in which transplant recipients receive both the needed organ and bone marrow from a living donor, producing a state called mixed chimerism, in which the patient’s immune system contains both donor and recipient elements. A number of patients have received kidney transplants using versions of this protocol – which is still considered experimental – and were subsequently able to discontinue immunosuppressive drugs. Most of these patients have been able to remain off immunosuppressive medications long term, some for more than a decade.
The current study was designed to test whether a similar protocol could induce tolerance to VCAs from immunologically mismatched donors in an animal model. An additional challenge is posed by the fact that skin, an essential part of a VCA, carries what could be considered its own immune system, making its acceptance by a recipient’s immune system particularly problematic. In several previous attempts to induce VCA tolerance, bone and muscle tissue were accepted but the skin was rejected and eventually separated from the underlying tissue.
Building on previous TBRC animal studies, the researchers tested whether combining bone marrow transplantation with VCA could induce chimerism and tolerance. In the first phase of the study, four recipient animals received bone marrow transplants from immunologically mismatched donors in advance, allowing time to confirm that chimerism had been established before the VCA procedure – involving transplantation of components of a hind limb from the same donor – was carried out three to five months later. Even though the recipients received no immunosuppression after the transplant procedure, all animals accepted the transplant with no sign of rejection.
Since pretransplant induction of chimerism would not be practical for hand or face transplants from deceased donors, the researchers tested VCA surgery conducted simultaneously with the bone marrow transplantation to induce tolerance in two recipient animals. Chimerism was successfully induced in both recipients, and overall results were the same as in the other group – immune tolerance of all components of the VCA with no evidence of rejection throughout the follow-up period, which for one recipient was more than 480 days.
In both groups of animals, the immune systems were preconditioned to accept donor immune cells prior to bone marrow transplantation. Since the availability of donor tissues cannot be precisely predicted, Cetrulo explains, the MGH team is exploring two approaches to the issue of timing the procedures. In one, immune conditioning begins as soon as a donor is identified and the transplant confirmed and continues during and immediately after a simultaneous bone marrow transplant/VCA procedure. The second adapts a protocol developed for organ transplantation in which the recipient receives conventional immunosuppression after VCA surgery and then immune conditioning and transplantation of donor marrow collected at the time of VCA are performed several months later.
“Along with investigating the role of skin-specific immunobiology in VCA tolerance, with the aim of identifying mechanisms that might by harnessed by clinical protocols of the future, we’ll be conducting preclinical evaluation of both of the tolerance preconditioning protocols, which if successful, could be ready for testing in a clinical trial within the next year,” says Cetrulo.