Finding could lead to new tumor immunotherapy targeting pivotal CTLA-4 protein
A major discovery that brings a new drug target to the increasingly exciting landscape of cancer immunotherapy was published yesterday by researchers from La Jolla Institute for Allergy and Immunology and their collaborators from other institutes.
The study, led by Amnon Altman, Ph.D., and Kok-Fai Kong, Ph.D., is particularly noteworthy because it reveals a new way to block the function of CTLA-4, an immune inhibitory checkpoint receptor already generating huge interest in the pharmaceutical and research communities due to its potential in fighting cancer. An antibody that blocks CTLA-4 is already in use for advanced melanoma.
“These important observations provide new insights into the mechanism of action of CTLA-4 and may provide a novel therapeutic approach against cancer,” says Dario Vignali, Ph.D., vice chair and member in the Department of Immunology at St. Jude Children’s Research Hospital, who studies immune-based approaches to cancer.
Mitchell Kronenberg, Ph.D., La Jolla Institute president & chief scientific officer, calls the discovery “an extremely important advance” that demonstrates a new way to boost the immune system’s ability to recognize and destroy tumors. “This is another example of the growing potential of the immune system as a new and powerful tool in the war on cancer,” says Kronenberg.
The finding was published in the prestigious journal Nature Immunology in a paper “Protein Kinase C-η Controls CTLA-4-Mediated Regulatory T Cell Function.” Altman, the La Jolla Institute’s director of scientific affairs, and Nicholas Gascoigne, who is a faculty member at Singapore National University and adjunct professor at The Scripps Research Institute in La Jolla, were co-senior authors. Kok-Fai Kong, an instructor in Altman’s lab, and Guo Fu, Ph.D., from the Scripps Research Institute were first co-authors. Additional scientists from the La Jolla Institute for Allergy & Immunology, the Scripps Research Institute and the RIKEN Center for Integrative Medical Sciences in Japan collaborated on this study.
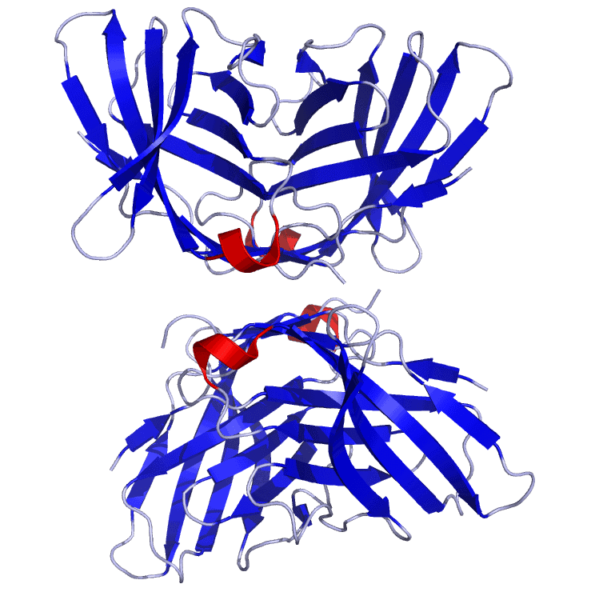
In the study, Altman and his team demonstrated a previously unknown – and pivotal — interaction between an intracellular enzyme Protein Kinase C-η (C-eta) and immune cell receptor CTLA-4 that is critical for the immune suppressive function of regulatory T cells. These cells are a subpopulation of T lymphocytes but, in contrast to most T cells, they suppress or turn down the immune system. This activity is an important component of a healthy immune system, where it serves to dampen exaggerated potentially harmful immune responses that lead to autoimmune diseases and other inflammatory conditions; however, on the flip side, regulatory T cells can also produce the undesirable effect of inhibiting beneficial immune attacks against cancer. CTLA-4 is a protein that sits on the surface of regulatory T cells, where it plays an important role in immune suppression. “The way it works is that this enzyme physically binds to the CTLA-4 receptor,” says Altman. “This binding is critical for certain suppressive functions of the regulatory T cells to proceed.”
Altman and his colleagues showed that binding of the enzyme to CTLA-4 was essential in order for the regulatory T cells to turn down the immune system in mice. Moreover, by eliminating the enzyme in specially-bred mice the research team also demonstrated that “regulatory T cells lacking this enzyme are unable to suppress the immune system’s response against a growing tumor,” says Altman.
Another key aspect of the study was the finding that, despite the failure of regulatory T cells lacking Protein Kinase C-η to inhibit an immune response against a growing tumor, these cells retained their ability to inhibit autoimmune disease in a mouse model of inflammatory bowel disease. “This means that you could potentially create a therapy that would allow for a more effective immune response against cancer without the risk of increasing susceptibility to autoimmune diseases,” says Altman. “This is quite desirable because it means the mechanism of action is more specific to tumors as opposed to unleashing an overzealous system-wide immune response that can trigger autoimmune diseases.”
Altman explains that this result was possibly due to diverse mechanisms utilized by regulatory T cells to suppress different immune responses. “At least some of the mechanisms that regulatory T cells use to inhibit autoimmunity seem not to depend on the association between Protein Kinase C-η and CTLA-4 and, thus, they remain largely operational in regulatory T cells that lack this enzyme,” says Altman. “The mechanism we discovered involves a physical contact between regulatory T cells and other critical immune system cells, which may be less important in the autoimmune pathways.”
Altman says his next steps will be to test the enzyme’s impact in models of additional autoimmune diseases and cancer, and to gain better understanding of how it controls the function of regulatory T cells. The La Jolla Institute is exploring potential industry collaborations to further develop this technology for translation into the clinic.