An early-stage clinical trial of an experimental Ebola vaccine conducted at the National Institutes of Health and the Walter Reed Army Institute of Research (WRAIR) found that the vaccine, called VSV-ZEBOV, was safe and elicited robust antibody responses in all 40 of the healthy adults who received it. The most common side effects were injection site pain and transient fever that appeared and resolved within 12 to 36 hours after vaccination. A report describing preliminary results of the NIH-WRAIR study appears online today in The New England Journal of Medicine. The VSV-ZEBOV candidate is one of two experimental Ebola vaccines now being tested in the phase 2/3 PREVAIL clinical trialthat is enrolling volunteers in Liberia.
“The ongoing Ebola ongoing outbreak in West Africa is unprecedented in scope and duration,” said Anthony S. Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases (NIAID), part of NIH. “The outbreak is slowly coming under control, thanks to extraordinary and multi-faceted efforts in the affected nations. However, there still are no licensed specific therapies or vaccines for Ebola. Until a safe and effective vaccine is available, the world will continue to be under-prepared for the next Ebola outbreak.”
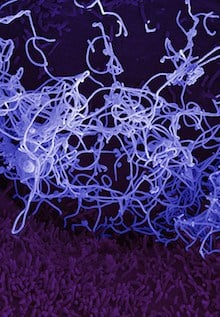
Scientists at the Public Health Agency of Canada developed the candidate vaccine. It was licensed to NewLink Genetics Corp. of Ames, Iowa, a company collaborating with Merck & Co. Inc., of Kenilworth, New Jersey, which is responsible for advancing this vaccine towards regulatory approval. The investigational vaccine is based on a genetically modified and attenuated vesicular stomatitis virus (VSV), a virus that mainly affects cattle. In the investigational vaccine, a gene for a VSV protein is replaced with a gene segment from a key protein in the Zaire species of Ebola virus. The vaccine does not contain the whole Ebola virus and therefore cannot infect vaccinated persons with Ebola.
The new report summarizes results of the first 52 volunteers enrolled in the study: 26 at the NIH Clinical Center in Bethesda, Maryland, and 26 at the WRAIR clinic in Silver Spring, Maryland. Six volunteers at each site received a placebo injection of saline solution, and the remaining 40 received the experimental vaccine at either one of two different dosages (2 x107 or 3 x106 in 20 volunteers at each site.) The NIH trial was led by NIAID investigators Richard T. Davey, Jr., M.D., and John H. Beigel, M.D., while Jason A. Regules, M.D., and Stephen J. Thomas, M.D., headed the trial at WRAIR.
The candidate vaccine’s ability to stimulate immune responses was assessed by sampling the volunteers’ blood at multiple time points following injection. (The blood sampling schedule differed between the two trial sites.) Of those volunteers tested at 14 days after injection, 93 percent (26 out of 28) of whose who had received vaccine developed antibodies against Zaire species of Ebola virus. Antibodies were detected in the remaining 14 volunteers who had received vaccine by 28 days after injection. Antibody responses were approximately three-fold greater in those who received the higher vaccine dose. This information was available to the designers of the PREVAIL trial and was used to guide the decision to use VSV-ZEBOV at the higher dosage level in that trial.
“The prompt, dose-dependent production of high levels of antibodies following a single injection and the overall favorable safety profile of this vaccine make VSV-ZEBOV a promising candidate that might be particularly useful in outbreak interventions,” said Dr. Davey.
The volunteers tolerated the vaccine well. Thirty percent (12 out of 40) of those who received the vaccine experienced mild or moderate fever; in all but one case, fever appeared and resolved within 24 hours of vaccination. The VSV-ZEBOV vaccine is made from live, weakened VSV and self-limiting fever following immunization with a live virus vaccine is not unexpected.
Some volunteers in a separate, Swiss study of this candidate vaccine reported experiencing arthritis that started in the second week after vaccination. Therefore, volunteers in the NIH-WRAIR study were specifically queried about new arthritis symptoms. No episodes of frank arthritis were reported by any volunteer.
More details about the NIH portion of this study are available at ClinicalTrials.gov using the identifier NCT02280408. Further details on the WRAIR portion are at ClinicalTrials.gov using the identifier NCT02269423.