A team led by Stanford University researchers has developed a wireless retinal implant that they say could restore vision five times better than existing devices.
Results in rat studies suggest it could provide functional vision to patients with retinal degenerative diseases, such as retinitis pigmentosa or macular degeneration.
A paper describing the implant was published online April 27 in Nature Medicine.
“The performance we’re observing at the moment is very encouraging,” said Georges Goetz, a lead author of the paper and graduate student in electrical engineering at Stanford. “Based on our current results, we hope that human recipients of this implant will be able to recognize objects and move about.”
Retinal degenerative diseases destroy photoreceptors — the retina’s rods and cones — but other parts of the eye usually remain healthy. The implant capitalizes on the electrical excitability of retinal neurons known as bipolar cells. These cells process the photoreceptors’ inputs before they reach ganglion cells, which send retinal signals to the brain. By stimulating bipolar cells, the implant takes advantage of important natural properties of the retinal neural network, which produces more refined images than the devices that skip these cells.
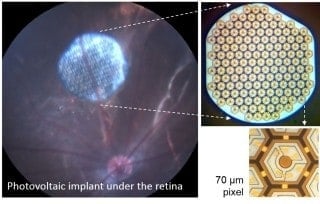
Made of silicon, the implant is composed of hexagonal photovoltaic pixels that convert light transmitted from special glasses worn by the recipient into electrical current. These electrical pulses then stimulate the retina’s bipolar cells, triggering a neural cascade that reaches the brain.
Clinical trial planned
So far, the team has tested the device only in animals, but a clinical trial is planned next year in France, in collaboration with a French company called Pixium Vision, said Daniel Palanker, PhD, professor of ophthalmology and a senior author of the paper. Initially, patients blinded by a genetic disease called retinitis pigmentosa will be included in the study.
Existing retinal prostheses are powered by extraocular devices wired to the retinal electrode array, which require complex surgeries, and provide visual acuity up to about 20/1,200. This new photovoltaic implant could be a big improvement because its small size, modularity and lack of wires enable a minimally invasive surgery. Vision tests in rats have shown it restores visual acuity to an equivalent of 20/250.
Next, Palanker and his team plan to further improve acuity by developing chips with smaller pixels. To ensure the signals reach the target neurons, they plan to add a tiny prong to each electrode that will protrude into the target cell layer.
“Eventually, we hope this technology will restore vision of 20/120,” Palanker said. “And if it works that well, it will become relevant to patients with age-related macular degeneration.”
Henri Lorach, PhD, a Stanford research associate, is the other lead author, and Alexander Sher, PhD, assistant professor of physics at the University of California-Santa Cruz, is the other senior author.
Other Stanford co-authors are Xin Lei, graduate student in electrical engineering; Theodore Kamins, PhD, consulting professor of electrical engineering; Philip Huie, PhD, senior research associate; and James Harris, PhD, professor of electrical engineering. The research was funded by the National Institutes of Health (grant R01EY018608), the Department of Defense, the NIH Clinical and Translational Science Award (UL1RR025744), the Stanford Spectrum fund, la Fondation Voir et Entendre and Pixium Vision. Information about the Department of Ophthalmology, which also supported the work, is available at http://ophthalmology.stanford.edu/.