Case Western Reserve University researchers today published findings that point to a promising discovery for the treatment and prevention of prion diseases, rare neurodegenerative disorders that are always fatal. The researchers discovered that recombinant human prion protein stops the propagation of prions, the infectious pathogens that cause the diseases.
“This is the very first time recombinant protein has been shown to inhibit diseased human prions,” said Wen-Quan Zou, MD, PhD, senior author of the study and associate professor of pathology and neurology at Case Western Reserve School of Medicine.
Recombinant human prion protein is generated in E. coli bacteria and it has the same protein sequence as normal human brain protein. But different in that, the recombinant protein lacks attached sugars and lipids. In the study, published online in Scientific Reports, researchers used a method called protein misfolding cyclic amplification which, in a test-tube, mimics the prions’ replication within the human brain. The propagation of human prions was completely inhibited when the recombinant protein was added into the test-tube. The researchers found that the inhibition is dose-dependent and highly specific in responding to the human-form of the recombinant protein, as compared to recombinant mouse and bovine prion proteins. They demonstrated that the recombinant protein works not only in the cell-free model but also in cultured cells, which are the first steps of translational research. Further, since the recombinant protein has an identical sequence to the brain protein, the application of the recombinant protein is less likely to cause side effects.
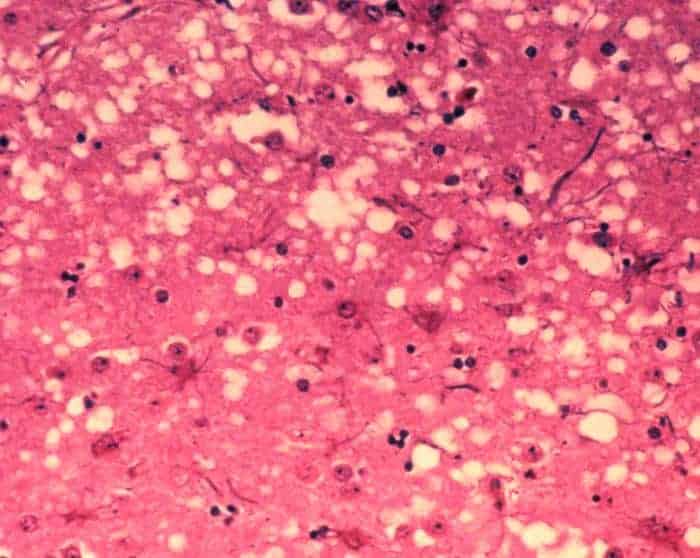
Prion diseases are a group of fatal transmissible brain diseases affecting both humans and animals. Prions are formed through a structural change of a normal prion protein that resides in all humans. Once formed, they continue to recruit other normal prion protein and finally cause spongiform-like damage in the brain. Currently, the diseases have no cure.
Previous outbreaks of mad cow disease and subsequent occurrences of the human form, variant Creutzfeldt–Jakob disease, have garnered a great deal of public attention. The fear of future outbreaks makes the search for successful interventions all the more urgent.
Zou, who also serves as the associate director of the National Prion Disease Pathology Surveillance Center at Case Western Reserve, and collaborators hope to extend their finding using transgenic mice expressing the human prion protein and patient-specific induced pluripotent stem cells (iPSCs)-derived neurons because they are made from human cells, offering an additional level of authenticity. The new animal models were generated in collaboration with Case Western Reserve School of Medicine faculty members, Robert Petersen, PhD, and Qingzhong Kong, PhD, who are the co-authors in this study. Further, patient-specific iPSCs-derived neurons have also just been generated in collaboration with fellow faculty, Paul Tesar, PhD, and Xin Qi, PhD.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!