A University of Colorado Cancer Center study recently published in the journal Cell Reports and presented today at the American Association for Cancer Research (AACR) Annual Conference 2014 shows that the cellular process of autophagy in which cells “eat” parts of themselves in times of stress may allow cancer cells to recover and divide rather than die when faced with chemotherapies.
Autophagy, from the Greek “to eat oneself,” is a process of cellular recycling in which cell organelles called autophagosomes encapsulate extra or dangerous material and transport it to the cell’s lysosomes for disposable. Like tearing apart a Lego kit, autophagy breaks down unneeded cellular components into building blocks of energy or proteins for use in surviving times of low energy or staying safe from poisons and pathogens (among other uses).
“What we showed is that if this mechanism doesn’t work right, for example if autophagy is too high or if the target regulated by autophagy isn’t around, cancer cells may be able to rescue themselves from death caused by chemotherapies,” says Andrew Thorburn, PhD, deputy director of the CU Cancer Center.
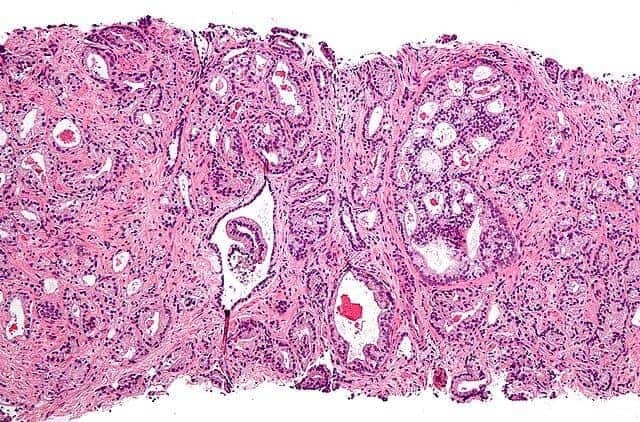
A movie that accompanies the study online shows a cancer cell dying. In the first few frames, mitochondrial cell walls break down and the cell’s mitochondria can be seen releasing proteins in a process abbreviated as MOMP, which is considered a common marker of cell death. But then high autophagy allows the cell to encapsulate and “digest” these released proteins before MOMP can keep the cell well and truly dead. Later in the movie, the cancer cell recovers and goes on to divide.
“The implication here is that if you inhibit autophagy you’d make this less likely to happen, i.e. when you kill cancer cells they would stay dead,” Thorburn says.
Thorburn and colleagues including postdoctoral researcher Jacob Gump, PhD, show that autophagy depends on the target PUMA to regulate cell death. Specifically, when PUMA is absent, it doesn’t matter if autophagy is inhibited because without the communicating action of PUMA, cancer cells continue to survive.
The finding has important implications. First, it demonstrates a mechanism whereby autophagy controls cell death. And second, the study further reinforces the clinical potential of inhibiting autophagy to sensitize cancer cells to chemotherapy.
“Autophagy is complex and as yet not fully understood,” Thorburn says. “But now that we see a molecular mechanism whereby cell-fate can be determined by autophagy, we hope to discover patient populations that could benefit from drugs that inhibit this action.”
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!