Chromosomal abnormalities that result in birth defects and genetic disorders like Down syndrome remain a significant health burden in the United States and throughout the world, with some current prenatal screening procedures invasive and a potential risk to mother and unborn child.
In a paper published online this week in the Early Edition of PNAS, a team of scientists at the University of California, San Diego School of Medicine and in China describe a new benchtop semiconductor sequencing procedure and newly developed bioinformatics software tools that are fast, accurate, portable, less expensive and can be completed without harm to mother or fetus.
“We believe this approach could become the standard of care for screening of prenatal chromosomal abnormalities,” said Kang Zhang, MD, PhD, professor of ophthalmology, founding director of the Institute for Genomic Medicine at UC San Diego and a staff physician at the San Diego VA Healthcare System.
The incidence of chromosomal abnormalities – in numbers or structure – is one in 160 live births in the United States, higher in other countries. In China, for example, the rate is one in 60 live births. The effects of these abnormalities, known as aneuploidies, can be severe, from developmental delays and neurological disorders to infertility and death. The incidence rate rises with maternal age, most notably after age 35.
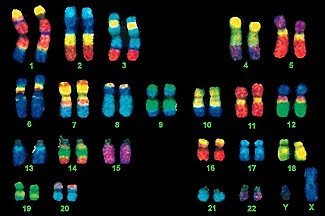
Current diagnoses of fetal aneuploidies often rely upon invasive tests that sample amniotic fluid or placental tissues for fetal DNA that can then be analyzed using a variety of complex and expensive methods, including full karyotyping in which the entire set of chromosomes is viewed microscopically. While highly reliable, these invasive tests may cause infections in the pregnant woman and pose as much as a 1 percent risk of miscarriage and fetal loss. Results are not available for one to two weeks, extending anxiety for families waiting for information.
The new method relies upon massively parallel sequencing of cell-free fetal DNA using a benchtop semiconductor sequencing platform (SSP) called an Ion Torrent sequencer developed by Life Technologies. Cell-free fetal DNA is genetic material from the fetus that circulates naturally and freely in the mother’s bloodstream. It can be obtained through an ordinary blood draw, with SSP analysis achieved in less than four days.
To assess the SSP method, researchers tested 2,275 pregnant women. More than 500 participated in a retrospective analysis, undergoing full karyotyping to establish known chromosomal abnormalities followed by SSP testing. The remainder participated in a prospective study without prior karyotyping, and SSP testing results were then compared to karyotyping results. The sequencing and automated bioinformatics analyses were performed at iGenomics in Guangzhou, China.
“We used the retrospective study to establish the method and the prospective study to validate it,” said Zhang.
In the retrospective study, the researchers found that SSP detected multiple types of chromosomal abnormality with virtually 100 percent sensitivity and specificity compared to full karyotyping.
“To our knowledge, this is the first large-scale clinical study to systematically identify chromosomal aneuploidies based on cell-free fetal DNA using SSP,” said Zhang. “It provides an effective strategy for large-scale, noninvasive screenings in a clinical setting. It can be done in hospitals and outpatient clinics, more quickly and cheaply.”
Co-authors are Can Liao, Fang Fu, Ru Li, Yong-ling Zhang, Yan-mei Ou, Jian Li and Dong-zhi Li, Guangzhou Medical University, China; Ai-hua Yi, Jie-xia Yang, Jing Wu, Ming-qin Mai and Xiao-zhuang Zhang, Guangdong Women and Children Hospital, China; Chun-fang Peng, Yang-yi Chen, Dong-hong Luo and Hai-liang Liu, iGenomics Co., Guangzhou, China; Rui Hou, Guangzhou Kang Rui Biological Pharmaceutical Technology Co, Guangzhou, China; Frances Wu, UCSD Institute for Genomic Medicine and UCSD Department of Ophthalmology; and Hongrong Luo, UCSD Institute for Genomic Medicine and UCSD Department of Ophthalmology and Sichuan University, China.
Funding for this research came, in part, from the National Natural Science Foundation of China, National Science Foundation for Young Scholars of China, National Natural Science Foundation of Guangdong, Key Project of Guangzhou Health Bureau, Major Project of Guangzhou Science and Technology and Information Bureau, 973 program and Burroughs Wellcome Fund.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!