Proof-of-concept study highlights new therapeutic use of engineered human stem cells
Harvard Stem Cell Institute scientists at Massachusetts General Hospital have devised a new way to use stem cells in the fight against brain cancer. A team led by neuroscientist Khalid Shah, MS, PhD, who recently demonstrated the value of stem cells loaded with cancer-killing herpes viruses, now has a way to genetically engineer stem cells so that they can produce and secrete tumor-killing toxins.
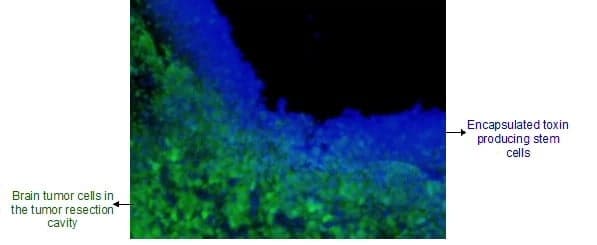
In the AlphaMed Press journal STEM CELLS, Shah’s team shows how the toxin-secreting stem cells can be used to eradicate cancer cells remaining in mouse brains after their main tumor has been removed. The stem cells are placed at the site encapsulated in a biodegradable gel. This method solves the delivery issue that probably led to the failure of recent clinical trials aimed at delivering purified cancer-killing toxins into patients’ brains. Shah and his team are currently pursuing FDA approval to bring this and other stem cell approaches developed by them to clinical trials.
“Cancer-killing toxins have been used with great success in a variety of blood cancers, but they don’t work as well in solid tumors because the cancers aren’t as accessible and the toxins have a short half-life,” said Shah, who directs the Molecular Neurotherapy and Imaging Lab at Massachusetts General Hospital and Harvard Medical School.
“A few years ago we recognized that stem cells could be used to continuously deliver these therapeutic toxins to tumors in the brain, but first we needed to genetically engineer stem cells that could resist being killed themselves by the toxins,” he said. “Now, we have toxin-resistant stem cells that can make and release cancer-killing drugs.”
Cytotoxins are deadly to all cells, but since the late 1990s, researchers have been able to tag toxins in such a way that they only enter cancer cells with specific surface molecules; making it possible to get a toxin into a cancer cell without posing a risk to normal cells. Once inside of a cell, the toxin disrupts the cell’s ability to make proteins and, within days, the cell starts to die.
Shah’s stem cells escape this fate because they are made with a mutation that doesn’t allow the toxin to act inside the cell. The toxin-resistant stem cells also have an extra bit of genetic code that allows them to make and secrete the toxins. Any cancer cells that these toxins encounter do not have this natural defense and therefore die. Shah and his team induced toxin resistance in human neural stem cells and subsequently engineered them to produce targeted toxins.
“We tested these stem cells in a clinically relevant mouse model of brain cancer, where you resect the tumors and then implant the stem cells encapsulated in a gel into the resection cavity,” Shah said. “After doing all of the molecular analysis and imaging to track the inhibition of protein synthesis within brain tumors, we do see the toxins kill the cancer cells and eventually prolonging the survival in animal models of resected brain tumors.”
Shah next plans to rationally combine the toxin-secreting stem cells with a number of different therapeutic stem cells developed by his team to further enhance their positive results in mouse models of glioblastoma, the most common brain tumor in human adults. Shah predicts that he will bring these therapies into clinical trials within the next five years.
This work was supported by the National Institutes of Health and the James S. McDonnell Foundation.
Cited: Stuckey, D. W. et al. Engineering toxin-resistant therapeutic stem cells to treat brain tumors. STEM CELLS. October 24, 2014. DOI: 10.1002/stem.1874
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!