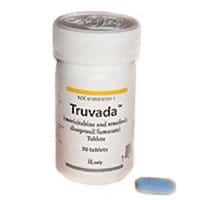
Women need daily doses of the antiviral medication Truvada to prevent HIV infection while men only need two doses per week due to the way the drug accumulates in different body tissues, according to a new study from pharmacy researchers the University of North Carolina at Chapel Hill.
The study, published in the Journal of Infectious Diseases, represents an important paradigm shift for HIV prevention strategies and could have major implications for clinical trial designs, said Angela Kashuba, Pharm.D., senior author of the study and the John and Deborah McNeill Distinguished Professor at the UNC Eshelman School of Pharmacy.
“Our data highlight the fact that one dose does not fit all,” Kashuba said. “In determining how best to use drugs to protect people from HIV, we need to understand where in their body they are at risk for being infected, along with the concentration of drug that is needed to protect that site from infection.”
Previous clinical studies showed that Truvada, the only prophylactic drug approved by the Food and Drug Administration to help prevent the spread of HIV, was more effective at reducing infection rates in men than in women, despite similar rates of drug adherence. Kashuba and her team are the first to explain the mixed clinical trial results by showing that different tissues require more or less of the drug to combat the virus.
The team shows that vaginal, cervical and rectal tissue all respond differently to Truvada. Twice as much of the drug is needed to prevent HIV infection in vaginal and cervical tissue than rectal tissue because fewer components of Truvada make it into those two tissue types. Also, there is more DNA material that the virus uses to reproduce present in vaginal and cervical tissues, thus requiring more of the drug to prevent infection.
“The more DNA material there is available for HIV to work with, the more medicine is needed to block the process,” said Mackenzie Cottrell, M.S., Pharm.D., a research assistant professor at the pharmacy school and lead author of the study. “In essence, we calculated the most effective drug-to-DNA ratio for each tissue type.”
The UNC-Chapel Hill team used human cells in a test tube to measure how much DNA material was in the cells and how much Truvada was needed to prevent HIV infection in these cells. Then they gave healthy female volunteers Truvada and measured how much of the drug got into vaginal, cervical and rectal tissue, and how much DNA material was there. Using both the test tube and human data, Kashuba and her team created a mathematical model that predicts the drug-to-DNA ratios in vaginal, cervical and rectal tissues and calculates the amount of drug needed to prevent HIV from infecting human tissues.
“We are excited to be able to apply our research methods to explain the conundrum of mixed clinical trial results of Truvada prevention, and how men and women should best use HIV prevention therapy,” Kashuba said. “Yet we would like to remind people who are taking pre-exposure prophylaxis that Truvada should be taken every day to reduce the risk of acquiring HIV infection. Patients should not change their medication regimen without first consulting their physicians.”
Daily dosing of Truvada was approved in 2012 to help prevent the spread of HIV, and it is the only drug approved by the FDA that has been shown to reduce HIV infection rates.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!