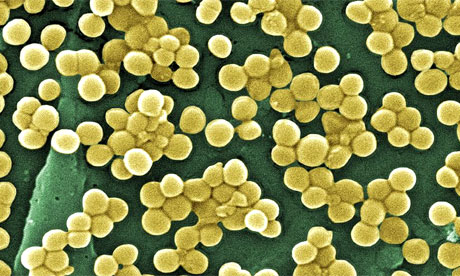
Scientists from the Center for Radiological Research at Columbia University Medical Center have shown that a narrow wavelength of ultraviolet (UV) light safely killed drug-resistant MRSA bacteria in mice, demonstrating a potentially safe and cost-effective way to reduce surgical site infections, a major public health concern.
A paper just published by PLOS ONE describes how the Columbia team found that a particular wavelength of UV light known as “far-UVC” (in this instance, 207 nanometers) is not only as effective as conventional germicidal UV light in killing MRSA, as shown in their previously published study, but also shows for the first time that, unlike conventional germicidal UV, far-UVC does not cause biological damage to exposed skin.
“Our new findings show that far-UVC light has enormous potential for combating the deadly and costly scourge of drug-resistant surgical site infections,” says David J. Brenner, PhD, the Higgins Professor of Radiation Biophysics, director of the Center for Radiological Research, and the senior author of the paper.
“We’ve known for a long time that UV light has the potential to reduce surgical site infections, because UV can efficiently kill all bacteria, including drug-resistant bacteria and even so-called ‘superbugs.’ Unfortunately, it’s not possible to use conventional germicidal UV light when people are around because it’s a health hazard to patients and medical personnel. What we showed in our earlier work is that far-UVC light is as effective at killing MRSA as conventional germicidal UV light—and now with this new research, we have demonstrated that far-UVC kills bacteria but without risk of skin damage,” Dr. Brenner says.
Surgical site infections (SSI) continue to be a critical health care issue in the United States and worldwide. Patients who develop SSI have a mortality rate twice that of non-infected patients, and estimated annual health care costs in the United States due to SSI range from $3 billion to $10 billion.
The new idea behind Columbia’s use of far-UVC light is that, unlike conventional germicidal UV, far-UVC cannot penetrate through the outer, dead layer of skin to reach live skin cells, nor can it penetrate the outer layer of the eye. However, because bacteria and viruses are physically very small, far-UVC light can penetrate and kill them. Columbia’s latest research was conducted on the skin of hairless mice, which responds similarly to human skin when exposed to UV light.
“Our findings offer a potential practical pathway towards significantly reducing surgical site infection rates without risk to the health and safety of patients and medical personnel,” adds Dr. Brenner. “One of our next steps is to explore direct studies in surgical settings, in larger animals and humans. From there we can investigate other new applications of these exciting findings, like killing airborne bacteria and viruses such as TB and influenza.”
“207-nm UV Light – A Promising Tool for Safe Low-Cost Reduction of Surgical Site Infections. II: In-Vivo Safety Studies” was published online on June 8, 2016, in PLOS ONE. Authors are David J. Brenner, Manuela Buonanno, Brian Ponnaiya, Alan W. Bigelow, Gerhard Randers-Pehrson, Yanping Xu, Igor Shuryak, and Lubomir Smilenov at the Center for Radiological Research, Columbia University Medical Center; Milda Stanislauskas at the Department of Dermatology, Columbia University Medical Center; and David M. Owens at the Departments of Dermatology and Pathology & Cell Biology, Columbia University Medical Center.
The Shostack Foundation and USHIO Inc. of Tokyo, Japan, provided funding for this research. USHIO has license and research agreements with Columbia University.
The authors declare no other conflicts of interest.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!