University of Colorado Boulder researchers have discovered a brain signature that identifies fibromyalgia sufferers with 93 percent accuracy, a potential breakthrough for future clinical diagnosis and treatment of the highly prevalent condition.
Fibromyalgia is commonly defined as chronic widespread musculoskeletal pain accompanied by symptoms such as fatigue, anxiety and mood disorders. The Centers for Disease Control and Prevention (CDC) estimates that fibromyalgia affects more than five million adults annually in the U.S., with significantly higher occurrence rates in women than in men.
Historically, fibromyalgia has been difficult to diagnose and treat due to a lack of a well-categorized tissue pathology and symptoms that overlap with other common chronic illnesses.
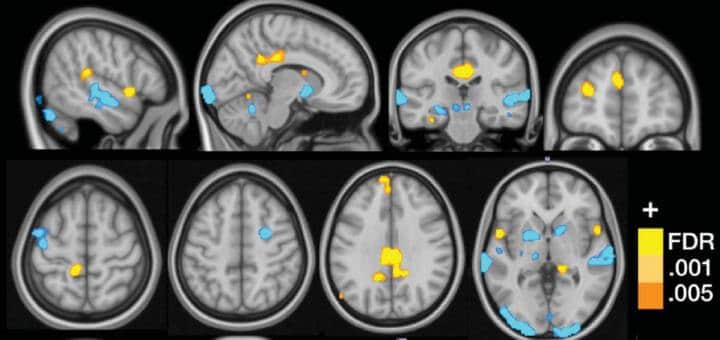
CU Boulder researchers used functional MRI scans (fMRI) to study brain activity in a group of 37 fibromyalgia patients and 35 control patients as they were exposed to a variety of non-painful visual, auditory and tactile cues as well as painful pressure.
The multisensory testing allowed the researchers to identify a series of three sub-markers, or neurological patterns, that correlated with the hypersensitivity to pain that characterizes fibromyalgia.
“The novelty of this study is that it provides potential neuroimaging-based tools that can be used with new patients to inform about the degree of certain neural pathology underlying their pain symptoms,” said Marina López-Solà, a post-doctoral researcher in CU Boulder’s Cognitive and Affective Control Laboratory and lead author of the new study. “The set of tools may be helpful to identify patient subtypes, which may be important for adjusting treatment selection on an individualized basis.”
The findings were recently published in the journal PAIN, published by the International Association for the Study of Pain.
“Though many pain specialists have established clinical procedures for diagnosing fibromyalgia, the clinical label does not explain what is happening neurologically and it does not reflect the full individuality of patients’ suffering,” said Tor Wager, director of the Cognitive and Affective Control Laboratory. “The potential for brain measures like the ones we developed here is that they can tell us something about the particular brain abnormalities that drive an individual’s suffering. That can help us both recognize fibromyalgia for what it is – a disorder of the central nervous system – and treat it more effectively.”
If replicated and expanded upon in future studies, the results could eventually provide a neurological road map to brain activity that would inform diagnosis and therapeutic interventions for fibromyalgia.
“This is a helpful first step that builds off of other important previous work and is a natural step in the evolution of our understanding of fibromyalgia as a brain disorder” said López-Solà.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!