A specific protein implicated in the cognitive decline of Alzheimer’s disease also appears to play a role in genetic predisposition to schizophrenia, meaning that a drug that targets that protein could treat a variety of neuropsychiatric disorders, according to a new study published October 18 in the journal Molecular Psychiatry.
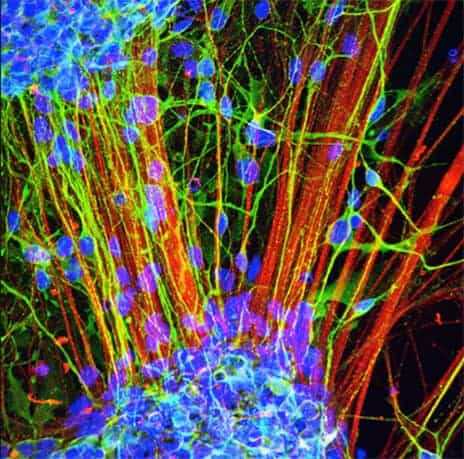
Yale researchers have been studying the role that the STEP (STriatal-Enriched protein tyrosine Phosphatase) protein plays in healthy functioning of synapses — the connections between brain cells. Excessive amounts of STEP protein are found in the brains of humans and animal models of Alzheimer’s disease, Parkinson’s disease, fragile X syndrome, and schizophrenia. The increase in STEP leads to a disruption of synaptic function and contributes to the cognitive deficits present in these disorders.
The research was led by Yale’s Paul Lombroso, the Elizabeth Mears and House Jameson Professor in the Child Study Center and professor of neurobiology and psychiatry, and Kristen Brennand at the Icahn School of Medicine at Mount Sinai.
In previous work, Lombroso and colleagues have shown that an experimental drug designed to inhibit the STEP protein restores cognitive deficits in a mouse model of Alzheimer’s disease. In the new paper, Lombroso shows that genetically eliminating STEP or using the drug to inhibit STEP activity improves cognitive deficits in a mouse model that has behaviorial features related to symptoms of schizophrenia. A team led by Brennand also found increased levels of STEP in human stem cells derived from skin cells taken from two groups of schizophrenia patients. A STEP inhibitor applied to those human stem cells corrected some of the biochemical and electrophysiological deficits that characterized these abnormal cells.
While the drug used in the earlier Alzheimer’s experiments has proven difficult to develop for clinical use, Lombroso said he and colleagues at Yale (professors Eric Ellman in chemistry and Angus Nairn in psychiatry) are developing new STEP inhibitors and, if successful, these may have more practical therapeutic value.
“These findings suggest that a STEP inhibitor, when discovered, may be the basis of a new drug that can treat a number of neuropsychiatric disorders,” Lombroso said.
Jian Xu of Yale and Brigham J. Hartley at the Icahn School of Medicine at Mount Sinai are co-lead authors of the paper.
The research was funded by the National Institutes of Health, the New York Stem Cell Foundation, and the Brain and Behavior Research Foundation.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!

A clinical trial being led by Queensland researchers is looking into whether the tropical fruit known as the Mangosteen could offer a gentler treatment for schizophrenia.
Mangosteen has long been used in traditional medicine in South-East Asia, and now Australian researchers hope to prove that its antioxidants could ease psychosis and other symptoms.
Mangosteen Fruit is one of the best antioxidants. Nutrients called Xanthones are most prevalent in the Mangosteen These Xanthones strengthen the cell walls, help fight against loose radicals and prevent infections from taking place. This process in turn enhances the immune system of the body and aids the metabolic activity. Xanthones may also help people maintain flexible joints and keep lungs healthy. The same anti-inflammatory benefits also contribute to reducing the problems associated with allergies. With Mangosteen Fruit Powder you get a concentrated amount without all the work of processing fresh fruit yourself and it’s great in smoothies. See Royaltropics.com. https://www.amazon.com/dp/B00A3N6USK