Orlando- In a significant advance in improving the safety of donor stem cell transplants, a major clinical trial led by researchers at Dana-Farber Cancer Institute and Brigham and Women’s Hospital (BWH) has shown that a novel agent can protect against the most common viral infection that patients face after transplantation.
The results represent a breakthrough in a decade-long effort to identify an effective drug for the prevention of CMV infection in transplant patients that doesn’t produce side effects that negate the benefit of the drug itself, the study authors said.
The findings, from an international phase 3 clinical trial of the drug letermovir for preventing cytomegalovirus (CMV) infection in transplant patients, will be presented at the 2017 Bone Marrow Transplant Tandem Meetings of the American Society for Blood and Marrow Transplantation (ASBMT) and the Center for International Blood and Marrow Transplant Research (CIBMTR) in Orlando, Florida, February 22, 2017.
The study, which involved 565 adult patients at 67 research centers in 20 countries, compared letermovir to placebo in preventing an active CMV infection following transplant with donor stem cells. The patients, who were undergoing transplant as treatment for blood-related cancers or other disorders, all carried a CMV infection from earlier in life that had been wrestled into dormancy by their immune system. Twenty-four weeks after completing up to 14 weeks of treatment, 61 percent of the patients receiving a placebo had developed a CMV infection serious enough to require treatment or had discontinued the trial. By contrast, only 38 percent of those treated with letermovir developed that level of CMV infection or did not complete the trial.
Unlike other drugs able to forestall active CMV infection in stem cell transplant patients, letermovir did so without producing unacceptable toxicities. Most of the side effects associated with letermovir were tolerable, including mild cases of nausea or vomiting, and some swelling, investigators found. Letermovir also conferred a survival benefit: at the 24-week mark, 15 percent of the placebo patients had died, compared to 10 percent of those receiving letermovir.
“For the first time, we seem to have a drug that is a true safe and effective preventive for CMV infection in stem cell transplant patients,” said the study’s lead author, Francisco Marty, MD, an infectious disease specialist at Dana-Farber and BWH. “Letermovir will allow many patients to avoid infection, usually with no or mild side effects, and seems to provide a survival benefit in the first six months post-transplant.”
Transplantation of donor hematopoietic stem cells – which give rise to all types of blood cells, including white blood cells of the immune system – is used to treat blood-related cancers such as leukemia, lymphoma, and myeloma, as well as several types of non-cancerous blood disorders. Patients typically receive chemotherapy to wipe out or reduce the bone marrow, where blood cells are formed, followed by an infusion of donor stem cells to rebuild their blood supply and reconstitute their immune system.
While refinements in transplant techniques have sharply improved the safety of the procedure, the reactivation of CMV infection following a transplant has been a longstanding problem.
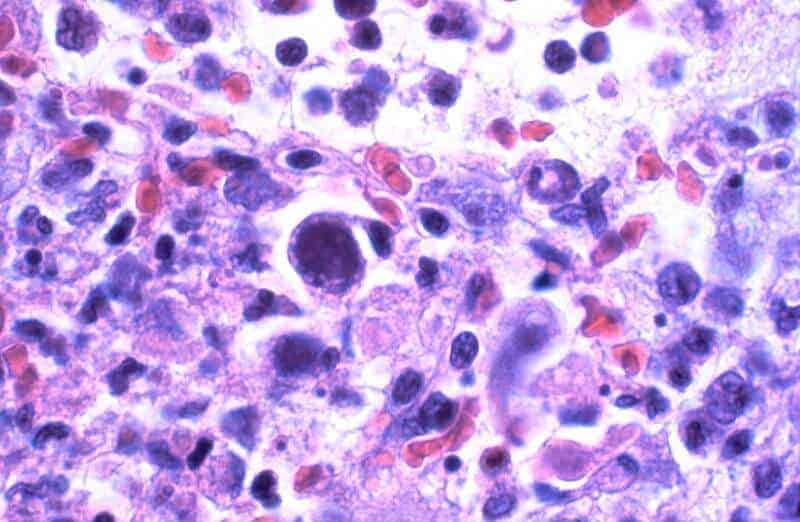
Infection with CMV, a type of herpes virus, is one of the most common viral infections in the world. In the United States, it’s estimated that over 50 percent of people are infected before adulthood. In other parts of the world, infection rates can be significantly higher. The effects of CMV infection can range from no symptoms to a flu-like fever or mononucleosis (“mono”) syndrome. Once the immune system has brought the infection under control, the virus persists unobtrusively in the body.
The jolt of a stem cell transplant – the rapid erasure or diminishment of the immune system produced by pre-transplant chemotherapy, as well as measures to prevent graft-versus-host disease – can give CMV a chance to reawaken and run amok before the newly reconstituted immune system takes hold. In the early years of bone marrow transplant therapy, 60 to 70 percent of transplant recipients developed CMV infection, Marty recounts. Of those, 20 to 30 percent contracted CMV pneumonia, and of those, 80 percent died of the disease.
In previous clinical trials, several drugs aimed at preventing CMV infection in stem cell transplant patients either were not effective or produced intolerable side effects. In the absence of safe preventive drugs, physicians worked out a “surveillance” approach in which they provide treatment only when patients develop CMV infection, and only for a short period of time. This strategy has largely been a success: patients now have just a 2 or 3 percent chance of getting CMV disease affecting the lungs or other organs. Still, the often harsh side effects of current drugs were reason to continue the search for a useful preventive agent.
Letermovir works by a different mechanism from previously tested agents, which block an enzyme known as DNA polymerase, which viruses use to duplicate their DNA. (Human cells use the same process to replicate their own DNA.) By contrast, letermovir blocks a process by which CMV is “packaged” inside infected cells – a wrapping that allows it to go on and infect other cells. The fact that this process does not occur in human cells may explain in part why letermovir usually gives rise to only mild side effects, researchers say.
In the trial, patients received letermovir or a placebo beginning an average of nine days after transplant. “The goal was to suppress the virus before it has a chance to become active,” Marty remarked. “The results of this trial offer encouragement that letermovir can offer a new strategy for donor stem cell transplant patients in preventing the emergence of CMV infection following transplant.”
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!