Up to 75 percent of patients with systemic lupus erythematosus—an incurable autoimmune disease commonly known as lupus—experience neuropsychiatric symptoms. But so far, our understanding of the mechanisms underlying lupus’ effects on the brain has remained murky.
In general, lupus patients have a broad range of neuropsychiatric symptoms, including anxiety, depression, headaches, seizures and even psychosis, said Allison Bialas, a Harvard Medical School research fellow in pediatrics at Boston Children’s Hospital. “But their cause has not been clear—for a long time, it wasn’t even appreciated that these were symptoms of the disease,” she said.
Perhaps, Bialas thought, changes in the immune system in lupus patients were directly causing these symptoms from a pathological standpoint.
Working with Michael Carroll, HMS professor of pediatrics at Boston Children’s, and other members of his lab, Bialas started out with a simple question. She soon made a remarkable discovery—one that points to a potential new drug for protecting the brain from the neuropsychiatric effects of lupus and other diseases.
The team’s findings were published June 14 in Nature.
How does chronic inflammation affect the brain?
Lupus, which affects at least 1.5 million Americans, causes the immune systems to attack tissues and organs. This causes white blood cells to release type 1 interferon-alpha, a small cytokine protein that acts as a systemic alarm, triggering a cascade of additional immune activity as it binds with receptors in different tissues.
Until now, however, these circulating cytokines were not thought to be able to cross the blood-brain barrier, the highly selective membrane that controls the transfer of materials between circulating blood and the central nervous system (CNS) fluids.
“There had not been any indication that type 1 interferon could get into the brain and set off immune responses there,” said Carroll, senior author on the paper.
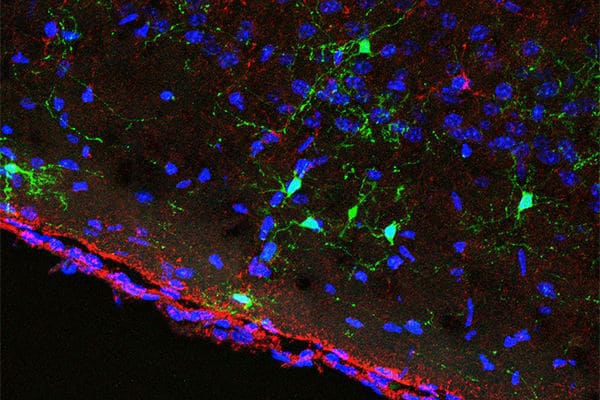
So, it was quite unexpected when Carroll’s team discovered in a mouse model of lupus that interferon-alpha did indeed appear to permeate the blood-brain barrier and cause changes in the brain. Once across the barrier, interferon-alpha launched microglia, the immune defense cells of the CNS, into attack mode on the brain’s neuronal synapses. This caused synapses to be lost in the frontal cortex.
“We’ve found a mechanism that directly links inflammation to mental illness,” said Carroll. “This discovery has huge implications for a range of central nervous system diseases.”
Blocking inflammation’s effects on the brain
The team decided to see if they could reduce synapse loss by administering a drug that blocks interferon-alpha’s receptor, called an anti-IFNAR.
Remarkably, they found that anti-IFNAR did seem to have neuroprotective effects in mice with lupus, preventing synapse loss when compared with mice who were not given the drug. What’s more, they noticed that mice treated with anti-IFNAR had a reduction in behavioral signs associated with mental illnesses, such as anxiety and cognitive defects.
Although further study is needed to determine exactly how interferon-alpha is crossing the blood-brain barrier, the team’s findings establish a basis for future clinical trials to investigate the effects of anti-IFNAR drugs on CNS lupus and other CNS diseases. One such anti-IFNAR, anifrolumab, is being evaluated in a phase 3 human clinical trial for treating other aspects of lupus.
“We’ve seen microglia dysfunction in other diseases like schizophrenia, and so now this allows us to connect lupus to other CNS diseases,” said Bialas, first author on the paper. “CNS lupus is not just an undefined cluster of neuropsychiatric symptoms, it’s a real disease of the brain—and it’s something that we can potentially treat.”
The implications go beyond lupus because inflammation underpins so many diseases and conditions, ranging from Alzheimer’s to viral infection to chronic stress.
“Are we all losing synapses to some varying degree?” Carroll asked. His team plans to find out.
This research was supported by the Alliance for Lupus Research (ALR – 332527), the National Institutes of Health (AI039246, AI42269, AI74549), MedImmune and the Jeffrey Modell Foundation.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!